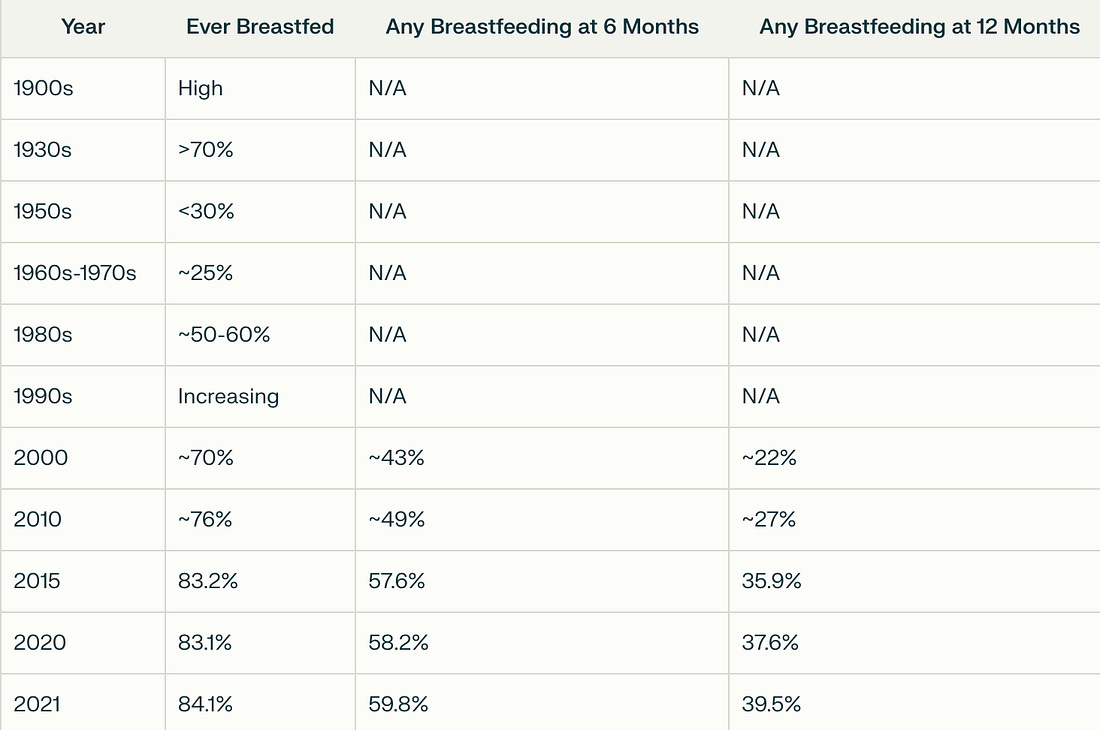
Why Is What We Feed Infants So Unhealthy?The Hidden Dangers of Infant Formula and The Incredible Benefits of Natural MilkStory at a Glance: •The infant formula industry has almost 100 billion dollars in annual sales. This was accomplished by unscrupulous marketing that trained doctors and parents to discard breastfeeding and tricked them into believing infant formula is “safe and effective.” •Infant formula is full of corn syrup and seed oils, which cause metabolic dysfunction and excessive weight gain. Remarkably, that weight gain has been normalized, making it possible to diagnose normal children as “underweight” and thereby push formula on them. •Infant formula is full of seed oils due to a 1980 law based on a 1963 study that concluded their fats were essential for development and hence must be in all formula. Since then, a mountain of evidence has emerged showing they’re actually harmful, but nonetheless, the 1980 formula requirements were never updated. RFK Jr. is thus the first H.H.S. Secretary ever to attempt to address this colossal mistake. •In contrast, breastmilk (alongside a healthy maternal diet) is one of the most nutritious substances an infant can consume, providing a myriad of benefits including developing the infant’s brain, gut, and immune system, decreasing many serious diseases, enhancing the critical mother-child bond, and reducing the mother’s risk of many severe illnesses (e.g., cancer). • Before the introduction of infant formula, mothers would often supplement their children’s diets with animal milks. If raw, these milks can yield significant benefits to children, while in contrast, when pasteurized, they have many issues (e.g., they frequently create allergies). •This article will review the critical points one must know to provide the most healthy nourishment for their child, how to navigate breastfeeding difficulties, and where to obtain the healthiest milk and infant formula. Three years ago, a nationwide infant formula shortage shook America, and before long led to fights at grocery stores and stories like this flooding the media: At the time, significant outrage was directed at the FDA since the shortage was due to pre-existing COVID-19 supply chain shortages exacerbated by a major recall by one of the leading formula producers (as at least two infants had recently died from contaminated formula, and the FDA had found the responsible bacteria at a major infant formula plant) which was then further exacerbated by a wave of panic buying that emptied many grocery stores. This then led to many people pointing out it was ridiculous the FDA was willing to pull America’s formula supply over a relatively small production issue, but simultaneously was unwilling to do anything about the mRNA vaccines despite the fact the contamination in them and the deaths they were causing were orders of magnitude greater than anything which could possibly be attributed to the suspect infant formula lines. As I watched this unfold, my thoughts were a bit different. Could there possibly be another way to feed your infants? Perhaps one that you could do at home that did not rely upon an unstable supply chain. I thus looked into how the homesteading and alternative health communities were addressing this dilemma and came across things like this: I thus took the events of 2022 as a remarkable testament to just how effectively the formula industry had convinced mothers they needed to do anything besides breastfeed their children. At the same time however, I was hopeful these events would catalyze a public shift on this issue, so since then, I’ve gradually tried to put out the key points needed to understand what’s gone awry with infant formula and facilitate that change. In turn, RFK Jr. recently announced an FDA initiative to make America’s infant formula healthy again (e.g., conducting a comprehensive review of its nutritional content, testing formula for heavy metals, and objectively assessing the health issues that arise from being formula fed). I believe that for “Operation Stork Speed” to succeed, it’s critical to understand the context of what’s happened with infant formula. Note: in addition to heavy metals (and other harmful chemicals), infant formula has also repeatedly been found to be contaminated with aluminum, something which is quite problematic due to its adverse effects on the physiologic zeta potential (which the nervous system is very sensitive to disruptions of). The History of Formula FeedingWhile I strongly believe in the value of breastfeeding, throughout history and cultures, there are many references of mothers who could not sufficiently nourish their children with breastmilk who then sought out milk from other mothers or other supplemental sources of infant nutrition (which unfortunately were often not nutritionally adequate or contaminated with microorganisms). Note: I believe that one of the primary causes of insufficient milk production from the mother was poor nutrition or malnutrition (something which was addressed in many early societies by having mothers eat specific diets). This led to a variety of attempts to create a milk substitute that more accurately matched the safety and efficacy of human breastmilk (starting in 1865), a process which was revolutionized through the discovery of evaporated milk powder and its adaptation into infant formulas in the early 1900s. That was followed by various other attempts to produce more nutritionally adequate formulas. As infant formulas improved in the 1920s, manufacturers began targeting physicians with their advertising. By 1929, the American Medical Association (AMA) established a committee to evaluate the safety and quality of formula compositions, leading many companies to seek the AMA’s “Seal of Acceptance,” bringing physicians closer to formula manufacturers. By the 1940s and 1950s, formula use became widely accepted as a safe alternative to breastmilk, and with the help of aggressive marketing and the inappropriate medicalization of childbirth, successfully displaced breastfeeding. Note: the AMA’s seal of approval was created in 1905, and was designed to be a source of revenue to keep the struggling organization afloat (as it was given in return for advertising dollars rather than any assurance of safety—for instance the AMA widely promoted the benefits of smoking their sponsor’s cigarette brand). Sadly, once this funding allowed the AMA to begin establishing a foothold in the medical market, the organization then switched to blacklisting every competing therapy which would not sell out to the AMA (which is essentially why there are so many remarkable forgotten medical therapies exist from the early 1900s). Many recognized this shift was harmful to both mothers and children. Hence, various groups (particularly the La Leche League, which was founded in 1956) mobilized the public to support breastfeeding mothers. In the 1970s, they finally reached the public (due to both scientific data emerging in support of breastfeeding and a growing societal dissatisfaction with the paternalistic and insensitive attitude medicine had to women). This shift began with middle-class mothers returning to natural breastfeeding, and gradually, governments eventually recognized the value of breastfeeding too (although it was not until 1984 that indecency laws against public breastfeeding began being updated). The decline in breastfeeding was, at last, reversed. One of the key events that catalyzed this shift away from formula was the Nestlé formula scandal (which began in 1973), which began after the public learned Nestlé was aggressively targeting poor women in undeveloped countries for infant formula sales. This was accomplish by paying hospitals to give free samples to mothers after delivery and telling mothers (frequently via sales reps impersonating nurses) that they would not be able to produce enough milk for their babies, which in turn let to the impoverished mothers frequently not only switching to infant formula but diluting it (as they could not afford standard doses). Millions of infants died as a result of these practices, and Nestlé eventually came under widespread public scrutiny (e.g., boycotts, celebrity protests, government investigations, and some of its predatory marketing practices being banned). The fact that Nestlé was able to convince millions of mothers to starve their babies to death again illustrates how predatory many of these marketing tactics were (particularly since some of those now outlawed practices still continue in the poorer nations). Formula MarketingDuring each pediatric “well-child” visit, in addition to pushing the currently scheduled vaccines on the child, the child will also be weighed and often told that, according to the growth chart, they are underweight, strongly encouraged to consume infant formula, and sent home with a free sample. One of the particularly concerning things for me about doctors pushing these products on children was that the ingredients in the most common brands were fairly unhealthy: Additionally, because of how frequently the “underweight” diagnosis came up, I naturally became quite suspicious of it. Note: somewhat analogously, patients will routinely be told that due to their blood pressure and cholesterol, they are at a high risk of having a heart attack in the next few years, so they must start a statin to prevent it. Given that almost everyone ended up being “high risk,” I was not surprised to learn that in 2016, Kaiser completed an extensive study which determined this calculator overestimated the rate of these events by 600%. Sadly, that has not deterred doctors from using this calculator (e.g., medical students are still tested on it for their board examinations). I then came across a passage from “How to Raise a Healthy Child In Spite of Your Doctor,” (written in 1987 by one of the original medical dissidents—Robert S. Mendelsohn) which stated the growth charts were extremely inaccurate (e.g., that they did not take into account a wide range of genetic variabilities in weight or that breast fed babies weighed less than formula fed ones) and that:
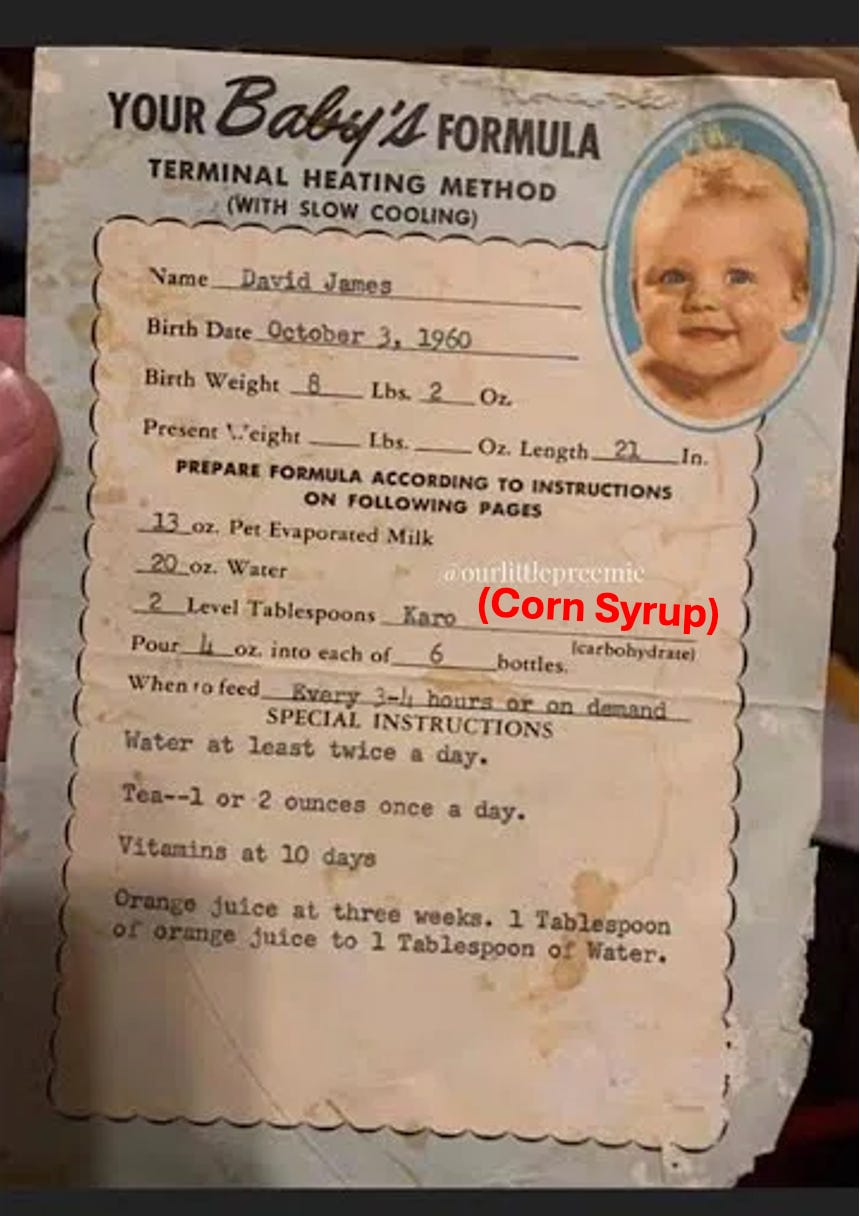
Thus, the scam was: •Infant
formula is composed of ingredients that will make children overweight
and obese (the first ingredient is often corn syrup and then followed by
seed oils). In turn, many studies (and systematic reviews) have found formula feeding not only causes rapid weight gain but also makes children much more likely to be obese as adults.1,2,3,4,5,6 As such, formula’s role in the continually increasing childhood obesity rates (e.g., 19.7% in 2020) must be considered (but unfortunately we are instead “solving” it by putting children on Ozempic—a drug which has a great deal of issues). Later, I got in touch with one of the (now retired) doctors Mendelsohn mentored, who shared a few other important things with me:
Fortunately, there is now growing awareness of the predatory tactics of the formula industry (which now has an annual growth rate of 10.15% and is a 90.91 billion annual market that costs the typical parent $1,500 to $2,500 a year). For example, to quote a recent investigation by the Lancet:
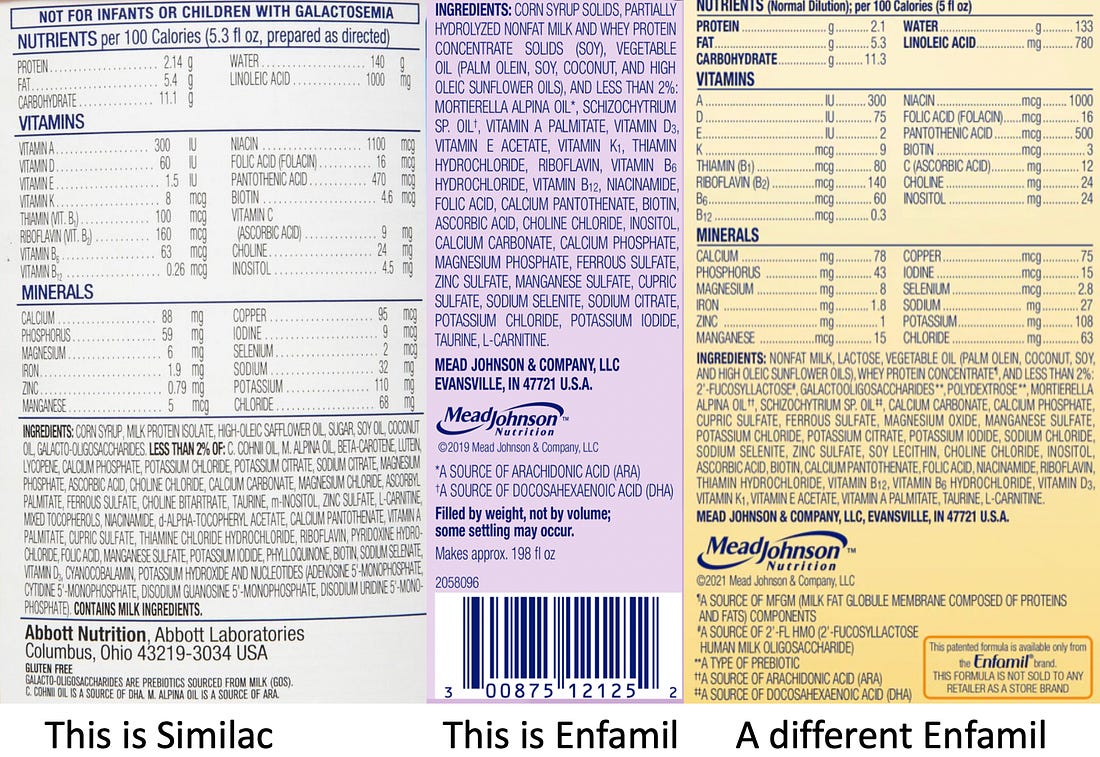
Note: the complete lack of evidence for many of the medical claims on infant formulas is discussed further here. Seed Oils In FormulaSince seed oils are linked to obesity, inflammation, and metabolic dysfunction, many parents do not want to give them to their children. In turn, I am frequently contacted by frustrated patients after they discovered that almost every infant formula is full of seed oils. After some digging, I discovered this remarkable situation (formula manufacturers refusing to sell the product customers want) was due to the following: •FDA
regulations require infant formulas to have at least 2.7% of their
calories (300mg per 100 Kcal) come from linoleic acid (LA, the problematic omega-6 fat in seed oils),
and the FDA aggressively enforces this. Additionally, no maximum is
given, so the amount of calories from LA in formula is often much higher
(e.g., 7-9% for many common brands and sometimes reaches 17%). •Those nutritional requirements were directly copied from the 1976 American Academy of Pediatrics (AAP) recommendations that did not provide an explanation for why the LA requirements were put in (which is odd given that LA was not mentioned in the AAP’s 1967 recommendations). •The Infant Formula Act had a provision [Section 412(a)(2)] that formula nutritional requirements could be revised at any time by the Secretary of the H.H.S. Remarkably, the only changes that were ever made were raising the minimum level of calcium per 100 kilocalories from 50 to 60 mg, phosphorus from 25 to 30mg and requiring 2.0-7.0 μg of selenium (which was instituted in 2016—27 years after the Institute of Medicine determined selenium was essential for children and formula manufacturers had already begun adding it in). So, as you might guess, nutritional science no longer supports many of the requirements in the 1980 act, but virtually all of that science has been completely ignored. In
the case of linoleic acid, (the omega-6 fatty acid), at the time the
act passed, the scientific consensus was that LA was essential for
infant development. This was due to data like a pivotal 1963 study of 428 infants
which found infants who had less than 0.1% of their calories come from
LA developed skin symptoms (e.g., drying, shedding, irritation, or
infections) due to a lack of oil in the skin (along with some degree of
“reduced growth”) which disappeared in those who instead received 1% of
their calories from LA. However, beyond the “necessary” amount of LA being much lower than what was subsequently required (2.7%) or what ended up in formula (e.g., the current brands I checked ranged from 7-17.1%), it also became obsolete after it was discovered that the ratio between LA to ALA (omega-3) was much more important than the LA present (e.g., too high of a LA to ALA ratio created significant issues, as did a lack of DHA). For example: •Those early studies did not include ALA in the experimental diets, and once a bit was present (e.g., 0.5%), the need for LA was halved. •High dietary LA has repeatedly been found to interfere with the synthesis, accumulation, and incorporation of fatty acids such as DHA.1,2,3,4,5
Likewise, decreasing the ratio of LA present was found to significantly
increase DHA in tissues, particularly the brain and retina.1,2 •One reason LA was considered “essential” is because the body converts it to arachidonic acid (ARA), which is critical for brain and nervous system development. However, in infants, the conversion is very poor (estimates range from 0.2-5%—this study for instance found infants only converted 1.2% of ingested LA to ARA), so infants require ARA rather than its LA precursor (e.g., 0.55% of the fats in human breastmilk are ARA). •High dietary LA does not support the growth of developing neurons, and in humans, it has been linked to atypical neurodevelopment and impaired motor and cognitive scores early in life. •High dietary LA increases the brain’s vulnerability to inflammation. In short, a strong case can be made that much of the original data arguing for the necessity of LA in formulas actually due to a lack of other essential fats, but rather than heed this, we opted to use an incredibly excessive amount of LA while simultaneously ignoring all of the science from the last 50 years that demonstrated the other fats needed to be focused on (and that, as a 2016 systematic review showed, we still have very poor data for these nutritional guidelines). Most remarkably, while other regulators (e.g., in China and Europe) have required fats like DHA to be included and lower LA to ALA ratios, the FDA has not (but will target companies who do not stuff their formulas with seed oils). Note: while the government will often be extremely stubborn and refuse to correct a longstanding mistake (perfectly demonstrated by this example), I strongly suspect the unwillingness to fix the linoleic acid requirements was significantly influenced by lobbying (as LA is one of the cheapest ingredients available to the processed food industry). Likewise, many believe the medical literature is so hostile to home formula options because industry money was spent to eliminate any potential competition. Milk in FormulasThroughout history, infants in many societies whose mothers could not produce sufficient milk have gotten supplemental milk (often mixed with water or supplemental grains) from a variety of animals (e.g., cows, goats, and sheep in many areas, water buffalos in parts of Asia, camels in the Middle East and North Africa, reindeers in northern Eurasia and llamas were a source of milk in South America. In America, prior to World War II, many textbooks advocated for feeding children raw animal milk and according to this author, mothers frequently would scout out a healthy cow to provide extra milk for their child and put it in the best available pasture. At the time pasteurization began to be implemented in milk in the late 1800s, it was arguably immensely valuable as while millions of children had been successfully raised on raw animal milks, children were also being sickened by microbial contaminated milk (as things were much less sanitary then than they are now and not every children had access to clean cow’s milk). As such, before long, a belief became entrenched that it was perilous to consume raw milk (mainly due to raw milk significantly increasing the risk of causing a listeria infection—something which can be quite dangerous to mothers, children, and the elderly). However, the data does not support that belief. For example, a (likely biased) 2003 risk assessment from the FDA
found many commonly consumed foods (that no one ever objects to) had a
much greater risk of causing a listeria infection than raw milk.
Similarly, a 2007 FOIA request
showed that from 1980-2005, there had only been three total cases of
listeria (all of which came from raw cheese not raw milk) and that all
other microbial infections (most of which aren’t that dangerous) were
also quite rare (typically under 100 per year). In contrast, when milk is pasteurized, a few significant issues occur due to the heat damaging specific vitamins and denaturing milk proteins. These include: •Enzymes (which provide a variety of essential health benefits) being lost. •Denaturing the proteins in milk turns them into allergens. In turn, we often find infants (along with many other age groups) will develop allergies from drinking pasteurized milk, but do not have those same issues with raw milk. Children raised on raw milk have fewer allergies, rashes, respiratory problems, and less asthma. Additionally: •While not ideal, evaporated (pasteurized) milk causes fewer allergy issues than liquid pasteurized milk. That said, it still can cause issues, and many infants who have difficulty tolerating powdered milk formulas have an excellent response to appropriately designed raw milk formulas. •Some people react to the A1 genetic variant (which is present in most milk and causes an inflammatory opioid peptide to be released when milk is digested). As such, consuming A2 rather than A1 milk in formula helps some infants (although typically it is not as impactful as having unpasteurized milk). •Some individuals (partly due to genetics) find goat’s milk easier to digest (and less reactive) than cow’s milk (but conversely goat’s milk is more likely to give infants constipation). Additionally, it is important to note that goat’s milk lacks folic acid and is low in vitamin B12, both of which are essential for growth and development and must be supplemented when feeding it to infants. •Some (but not all) lactose-intolerant individuals can digest milk if it is raw rather than pasteurized. Note: many of these issues originated from a very popular 1946 textbook which overturned the previous emphasis in pediatrics on raw milk and healthy animal fats, arguing they should be replaced with “easier to digest” evaporated milk products and processed carbohydrates. Sadly, this bias against critical fats never went away, and many authoritative books on child-raising still warn against it (whereas in contrast they often aggressively promote raising children on soy). In contrast to milk, the other popular approach has been to give infants a plant-based milk substitute (e.g., soy milk). Many (myself included) do not endorse this approach as plant-based “milks” are lacking in many of the essential fats and nutrients found in animal milks and often contain problematic additives.1,2 Note: before the rise of plant “milks,” Gerber sold a meat-based formula for babies who could not tolerate milk-based formula (while now a few nutritionally adequate home recipes exist to produce meat-based home formulas). Of the plant “milks,” soy milk is particularly problematic due to the high amount of phytoestrogens soy puts into the bloodstream, soy’s effect on thyroid function, soy’s frequent contamination with other chemicals (e.g., herbicides), and soy’s tendency to block the absorption of many critical nutrients. The Benefits of BreastmilkOne of the most reliable approaches for creating a successful business is to replace something (free) that people rely upon with a patentable product. Unfortunately, when this happens, the synthetic substitute is often a meager shadow of what it replaces. In turn, while many attempts have been made to make formulas that are closer in nature to breastmilk, they still frequently fall short as human breastmilk is an immensely complex substance. For example, it contains a variety of complex bioactive molecules which allow the mother to continually aid the growth and health of their child such as: •Numerous vital growth factors (e.g., ones that facilitate the development of the gastrointestinal tract,1,2,3,4). •A unique set of antibodies and immunoglobulins are produced by the mother to both protect the infant against expected pathogens in the environment (e.g., what the mother has encountered) while the infant’s immune system is still developing, and guide the development of their immune system. •Key
cytokines such as TGF-β, IL-6 and IL-10 which also play a critical role
in much of the previous (e.g., promoting oral tolerance, supporting
immune system development, and enhancing intestinal epithelial
proliferation and repair).1,2,3 •A variety of enzymes that both help the infant’s digestive tract break down the ingested milk and release key peptides from breastmilk components (that both develop the immune system and directly eliminate pathogenic organisms),1,2,3 along with many other enzymes and bioactive molecules that inhibit microbial growth (e.g., lactoferrin, lysozymes and mucin, interferon and fibronectin). •A protein with potent anticancer activity (against over 40 types of cancers) that does not harm normal cells and has successfully treated cancer in humans. It also has powerful antimicrobial activity (particularly against streptococcal bacteria) and enhances bacterial sensitivity to antibiotics (including in antibiotic resistant bacteria). •Breastmilk contains endogenous cannabinoids that are important for human development (e.g. by affecting appetite, mother-child bonding, immune function, brain development and motor function). Note: the most potent milk a mother releases is the colostrum (the first milk). In parallel, over the years, many have discovered that colostrum from healthy cows has healed a variety of challenging illnesses and significant injuries (which is detailed in this book). Furthermore, breastmilk also contains a variety of nutrients which are invaluable for the developing infant such as: •Human Milk Oligosaccharides that support the growth of healthy gut bacteria (e.g., bifidobacteria and lactobacilli), reduce inflammation, and contribute to immune system development. •Containing essential fatty acids, cholesterol (and many other unique lipids) which are critical for brain development, eye development, and cognitive function (e.g., academic success). These fats are not present in infant formula (or present in relatively low levels—except in animal milk substitutes, as it’s well recognized copious fats are necessary for their growth) and many experts in the field believe
their absence from formula is one of the reasons why breastmilk is so
much healthier for infants. Human breastmilk also contains bile salt-stimulated lipase,
an enzyme absent in cow’s milk and most other commonly consumed milks
(e.g., formula) which is specifically adapted to enhance the digestion
and absorption of fats and cholesterol in human infants. •Highly bioavailable nutrients (e.g., iron), which allows much lower concentrations of them needed in milk than formula (which then prevents those nutrients from competing with the absorption of other critical nutrients, such as iron added to infant formula interfering with the critical absorption of zinc). Note: if breastmilk (or formula) is stored, it should never be microwaved to warm it (as this destroys many critical nutrients). Likewise, most sources of donated human breastmilk will pasteurize them (which destroys many of these vital components in milk). In short, I would argue that the complexity of breastmilk makes it unlikely a synthetic substitute will ever be able to replace it (e.g., many of the bioactive molecules it contains cost thousands of dollars to synthesize). In turn, beyond being less likely to be overweight or have a dysfunctional metabolism (e.g., one study found breastfeeding halved the risk of diabetes), many other benefits have also been attributed to breastfeeding such as: •Lower rates of infections (e.g., pneumonia, ear infections) and lower hospitalization rates (e.g., for infections). •Lower rates of gastrointestinal issues (e.g., stomach problems, constipation, gas, diarrhea) and allergies (e.g., being half as likely to develop asthma). •Being half as likely to die from Sudden Infant Death Syndrome (a condition decades of evidence shows is linked to vaccination). •Being less likely to develop cancers (particularly leukemia). •Improved brain development (particularly white matter growth). •Improved cognition (e.g., verbal and spatial skills or mathematical ability and working memory). Likewise, breastfeeding for 12 months was associated with a three-point increase in IQ (along with a 0.8 point increase for each additional month), and higher educational and financial success in life. •Being significantly less likely to develop autism or ADHD. Note: many of the conditions breastmilk prevents often follow vaccination. Breastmilk’s ability to prevent those conditions is likely due to it reducing the Th2 response, improving the physiologic zeta potential, and reducing the total allergen burden seen with formula feeding (as consuming allergens exacerbates existing autoimmune processes). Breastfeeding also offers significant benefits to the mother, both immediately after pregnancy and later in life. In the short term, it promotes better infant bonding, enhances maternal mood, aids in post-pregnancy weight loss, and reduces the likelihood of developing postpartum depression.1,2 Over the long term, in addition to each childbirth lowering the risk of breast cancer by 7%, breastfeeding over 12-months of breastfeeding reduces the risk of breast cancer by 4.3%, ovarian cancer by 34% (and by up to 91% with extended breastfeeding), as well as decreasing the risks of endometrial cancer and high blood pressure. Early FeedingAs I show here, many of these benefits attributed to breastfeeding are also seen in mothers who avoid the more invasive (and often unnecessary) hospital birth procedures. It hence should come as no surprise that mothers who undergo invasive birthing procedures are significantly less likely to breastfeed—which again illustrates the critical need for our society to reexamine how we handle bringing our children into this world and raising them. For
example, skin-to-skin contact (which is often is prevented at hospital
births) provides many immense benefits to infants (including make them
less likely to cry1,2,3,4)
and to their mothers including stimulating the a critical maternal
release of oxytocin (a hormone necessary for lactation), and in one study
infants separated from their mothers during the first week of life were
half as likely to breast feed (37% vs. 72%). Newborns infants are eager
to latch in the first 30 minutes following birth and this early period
is critical for both the infant (e.g., to set the rhythm of feeding and
to obtain the mother’s colostrum which is only present for a few days
after birth) and the mother (as the maternal oxytocin release from
suckling helps to expel the placenta, contract the uterus, and hence
minimize postpartum blood loss). For these reasons, it is critical to
ensure this early feeding occurs over the first several days of the
child’s life, and if possible not to introduce any artificial nipples
(e.g., pacifiers or bottles) during that time. Likewise, analgesia during childbirth or delaying the start of breastfeeding has been shown to impair the ability of the infant to breastfeed. Because of this, it’s important to be informed about the hospital birthing process before you arrive, have appropriate support while there, and if at all possible, to deliver at a “baby friendly” hospital. Note: one popular practice is to wrap infants in blankets to soothe them, prevent them from moving and help them get to sleep. While this practice is viewed as safe if done correctly (which it often is not) I am not a fan of swaddling infants as I feel they should be moving, swaddling has repeatedly been linked to doubling the risk of sudden infant death, developmental hip dysplasia, overheating the baby, and breast feeding—particularly if the infant is swaddled immediately after birth. Healthy BreastmilkWhile a significant body of evidence shows breastfeeding is much better for infants, other studies show formula gets comparable results to breastfeeding. This discrepancy can likely be attributed to the fact that breastmilk production is highly dependent upon maternal nutrition. For example, one of the reasons why linoleic acid was deemed “essential” was due to LA’s presence in breastmilk, but its presence is a product of how much dietary LA is consumed, and over the last 50 years (in tandem with increasing seed oils flooding the food supply), LA levels in human breastmilk have roughly tripled (while ALA levels have remained the same). As such, if mothers are eating a healthy diet full of the fats and nutrients that are needed for infants (e.g., fat soluble vitamins and B12) they will produce significantly better quality breastmilk, whereas in contrast if the mother consumes junk food, nutritionally inadequate foods (which frequently becomes an issue in vegan breastfeeding mothers), unhealthy fats (e.g., trans fats or partially hydrogenated vegetable oils—both of which have been repeatedly shown to reduce healthy fats in breastmilk and are not put into infant formula), or other forms of junk food, the quality of their breastmilk will be dramatically less nourishing for the baby (and in some cases, the baby’s dissatisfaction with those unhealthy fats will cause them to stop nursing and a frustrated mother to switch to formula). As such, if mothers eat a healthy diet rich in essential fats and nutrients (e.g., fat-soluble vitamins and B12), they will produce significantly better-quality breastmilk. On the other hand, if the mother consumes junk food or nutritionally inadequate foods, especially common among vegan breastfeeding mothers, the quality of her breastmilk will suffer. Additionally, consuming unhealthy fats (e.g., trans fats or partially hydrogenated oils,) has been repeatedly shown to reduce healthy fats in breastmilk, making the milk less nourishing and sometimes leading the baby to stop nursing and the exasperated mother then switching to formula. Consequently, we frequently observe that infants brought up on an optimal diet (either from a natural formula or healthy breastmilk) tend to be healthier and more vibrant than their peers. In turn, one of the strongest motivating factors for someone to take charge of their health is to do so for their children and in many cases, we used a new life entering the family as a way to motivate parents to initiate the health changes they kept putting off (e.g., if at all possible, for both the mother and her infant, a healthy organic diet should be adopted by the mother). Note: one of the best resources I have come across to provide guidance to mothers for nourishing their developing children (e.g., for producing nutritionally optimal breastmilk) is Nourishing Traditions, a book that draws upon the traditional practices many cultures used to raise healthy children (as again and again, Weston Price discovered once modern diets were introduced to them, poor skeletal development, facial development, and chronic illness were observed in the populations that could be directly tied to key nutritional deficiencies such as a massive loss of dietary Vitamin A, D and K₂—all of which in tandem have greatly declined within human breastmilk). Many within the holistic field in turn believe the loss of these critical nutrients from animal fats is a root cause of the chronic illness our society face (e.g., fat soluble vitamin A is important for infant development, is not found in breastmilk without adequate dietary sources and has been found to frequently be deficient in thin women or those who had babies too closely together without adequate prenatal supplementation). Likewise, improper skeletal development can lead to a variety of other issues (e.g., poor development of the cranial bones impairs drainage from the head and Price found tonsillitis, ear infections and sinusitis were extremely rare in children whose traditional diets facilitated a proper development of the cranium). One
of the least appreciated aspects of breastmilk is that whatever the
mothers consumes will frequently make its way into the breastmilk (e.g.,
dietary peanut allergens, COVID vaccine antibodies and vaccine mRNA have been all found in breastmilk and there are many reports of children having significant reactions to breastfeeding from a recently vaccinated mother). As such, we frequently observe that mothers consuming certain foods (particularly chocolate and pasteurized milk products, and also often eggs, gluten, MSG, or soy) can trigger reactions in infants (e.g., crying, poor digestion or rashes). As such, it is important to monitor an infant’s reaction to breastmilk and see if it correlates with certain foods the mother eats. Similarly, many environmental toxins can also concentrate in breastmilk (e.g., pesticides and flame retardants). Likewise, certain medications can be unwise to take while breastfeeding (e.g., hormonal birth control can suppress milk production and transfer into milk). Note: if a grain the mother consumes causes issues for infant, organic, fermented, soaked, or pressure cooked versions of that grain can sometimes be tolerated. Simultaneously, beneficial substances are also concentrated in breastmilk. Iodine for example
(which is necessary for thyroid function) is essential for normal
growth, mental development, and survival of infants. It is thus present
in breastmilk at levels 20-50 higher than that found in the mother’s plasma. As such, a significant focus has gone into preventing consequential maternal iodine deficiencies
(which are quite common), and likewise, some women with deficient
iodine or thyroid hormone levels will not be able to produce breastmilk
until their iodine deficiency is corrected. Lastly, one of the most common issues parents deal with is “colic” (frequent crying or fussiness for no apparent reason), which is often treated as an inconsequential issue (“it’s just colic”). The cause of colic is generally a mystery, but it is usually viewed to be linked to some type of (unspecified) digestive issue causing discomfort. I personally believe “colic” compromises two entirely different conditions—vaccine encephalitis (which is characterized by a sharp piercing cry) versus a variety of (painful) issues in the GI tract or the infant still being hungry after feeding. In those cases, it is frequently due to the wrong food being fed to the infant (e.g., an unhealthy formula or allergen containing breastmilk). It can often be corrected by giving the correct food or removing the allergen from the mother’s diet (or specifically in breast-fed children, by providing the correct [infant-designed] probiotic1,2,3,4). Note: since childhood, I noticed the encephalitic cries many babies would make (as their piercing quality felt both unnatural and indicative of something being genuinely wrong within the baby). Later, when I began learning about the dangers of vaccination, I concluded what I was sensing had to be some type of vaccine brain injury and eventually discovered this was indeed the case (e.g., as many mothers had noticed it start after a vaccine injury and that type of cry has long been linked to encephalitis and encephalitis causing vaccines). It hence always surprised me that virtually no recognition of this issue exists within the medical field (rather it’s just something inconsequential like “colic”) and I always feel bad for the babies I run into exhibiting it (particularly since to some extent I not only hear but feel the pain within those cries). Breastmilk DifficultiesOftentimes,
when something is meant to happen, the collective consciousness shifts
towards making it a reality, and multiple parties independently decide
to take action toward it. For example, in December I suddenly felt I
needed to put together a series about the mistakes we repeatedly make
around childbirth (e.g., prenatal care, pregnancy ultrasounds and hospital birthing)
that would seed the idea there were major problems with the 1980 infant
formula act and culminate in this piece about early nutrition because
of just how impactful it is on the entire life of a child. In turn,
Kennedy’s team came to the same conclusion and hence made a large scale
operation (Operation Stork Speed) to tackle this one of their key
priorities. The
confluence of these events illustrates that we are very close to a
societal shift on this subject. However, while many now recognize the
value of breastfeeding, many mothers nonetheless are unable to
breastfeed their infants. As such, mothers must be given the proper
support to nourish their children (e.g., lactation consultants can be
beneficial, and we often advise patients to contact their local La Leche League group leader). Similarly, one of the most important,
but frequently missed points in this area, is that the mother needs to
be supported as much as possible during the post-delivery process (e.g.,
with maternity leave and a supportive family), notably since stress
(particularly chronic stress) frequently significantly decreases milk production. In
contrast, if a mother’s well-being is prioritized, the other necessary
areas (e.g., the marriage and the infant's health) tend to work
themselves out. In the second part of this article, I will discuss the most useful strategies we have found over the years for allowing mothers to lactate, address feeding difficulties (e.g., insufficient milk production, poor infant latching, mastitis or sore nipples, colic, when to wean etc.) along with the best resources I’ve found for obtaining healthy infant formula or clean raw milk... Continue reading this post for free in the Substack app |


No comments:
Post a Comment