The Innate and Adaptive Immune Systems, The Vaccine and Spike Protein
Immune senescence, Christian theology, and the Spike protein
One of the things that happens to our immune systems with age is that a preponderance of naïve B-cells (in youth) gives way to a diverse body of memory B-cells (in older adults), each trained to respond to a specific pathogen from the past. (Valter Longo claims that fasting eliminates some of the memory B-cells, which are replaced by naïve B-cells upon re-feeding.)
We know that old and young people have very different responses to COVID and to the COVID vaccines. There is a link between the B-cell story and the differential responses of old and young if we look at a recently re-discovered phenomenon called original antigenic sin. (The term was coined in a 1960 article on influenza.)
The innate immune system is our first and best line of defense. It is strongest in youth. Neutrophils engulf and digest bacteria and viruses. In addition to neutrophils and natural killer cells, there are short proteins in mucus membranes that protect us.
The mucus layer also contains substances that kill pathogens or inhibit their growth. Among the most abundant of these are antimicrobial peptides, called defensins, which are found in all animals and plants. They are generally short (12–50 amino acids), positively charged, and have hydrophobic or amphipathic domains in their folded structure. They constitute a diverse family with a broad spectrum of antimicrobial activity, including the ability to kill or inactivate Gram-negative and Gram-positive bacteria, fungi (including yeasts), parasites (including protozoa and nematodes), and even enveloped viruses like HIV. Defensins are also the most abundant protein type in neutrophils (see below), which use them to kill phagocytosed pathogens. It is still uncertain how defensins kill pathogens.
—Molecular Biology of the Cell, 4th Edition
How do these simple, generic defenses distinguish invaders from self? There are certain molecules that are characteristic of bacteria and absent in eukaryotes.
The pathogen-associated immunostimulants are of various types. Procaryotic translation initiation differs from eucaryotic translation initiation in that formylated methionine, rather than regular methionine, is generally used as the first amino acid. Therefore, any peptide containing formylmethionine at the N-terminus must be of bacterial origin. Formylmethionine-containing peptides act as very potent chemoattractants for neutrophils, which migrate quickly to the source of such peptides and engulf the bacteria that are producing them….Short sequences in bacterial DNA can also act as immunostimulants.
—Mol Biol of Cell, 4th Ed
Innate immunity is based on inflammation. I’ve seen several sources that describe how the brilliant, all-purpose system of innate immunity turns to chronic, un-targeted inflammation with age, but no explanation as to how the inflammatory response loses its way and attacks the body generally.
The great resistance that young people have to the COVID virus seems to be due to a strong innate immune system; conversely, the second line of defense, the adaptive immune system, which older people rely on, seems to have more trouble with COVID.
Original antigenic sin (OAS): When the immune system first encounters a pathogen, a tiny subset of randomly-generated antibodies that happens to match a subregion (about 120 AA bases) of some protein in the invader is copied in an exponential process that leads to enormous amplification. Thereafter, the body has a memory of some protein fragments of the pathogen, but not others. When the same pathogen is detected months or years later, the immune system will favor its remembered response, rather than exploring its naïve cells for a new one.
The problem called “original sin” arises when the new invader is a related pathogen, not identical to the one first encountered. The immune system recognizes some subsequences, and figures, based on its memory, “we’ve got this one covered”. But sometimes the response that worked well with the original pathogen is sub-optimal for the new one. The body may fail to fight off a new virus simply because it has encountered a similar one in the past. This is the phenomenon that Thomas Francis dubbed “original sin”.
The relevance to present-day pandemic epidemiology is this: Coronaviruses are ubiquitous, and have been around longer than humans; we have all been exposed to many of them. When our bodies first encounter SARS-CoV-2, they are likely to yawn and say, “this looks a lot like something I’ve seen before”. And indeed, this seems to work well for a lot of bodies. No less a light than John Ioannidis has estimated that up to 80% of people cast off the COVID virus with symptoms so mild that they never know they had it. But there are other people for whom the remembered response to some generic coronavirus is not sufficient, and their immune systems get stuck in an obsolete paradigm. Original sin.
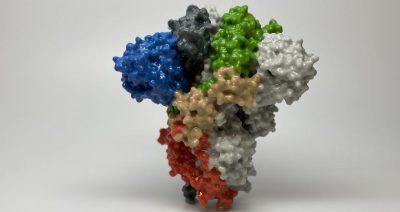
“Original sin” can apply to vaccines as well. The COVID spike protein binds to the ACE2 receptor, and has this in common with spike proteins from many past coronaviruses. This makes it likely that parts of the SARS-CoV-2 spike protein have similar regions to other common coronaviruses from the past, (including the original 2003 SARS). The spike protein, of course, is the element of the virus that was chosen by all Western vaccine manufacturers to induce with their vaccine products. So we see a possible reason why young people and old people have such different reactions to the vaccine: young people are responding to the vaccine from the innate immune systems, while older people are responding by selectively amplifying antibodies from their immune memory.
Age and Vaccine Side Effects
The current crop of mRNA vaccines have caused in 11 months about twice as many adverse reactions, including deaths, as the total of all previous vaccines in the 30-year history of VAERS. These post-vaccination events deserve to be counted and addressed. CDC is in denial.
Reported heart attacks (9,746 cases) and deaths (19,532) after vaccination are skewed toward older people. The average age for heart attacks is 62. [these numbers from OpenVAERS]

Myocarditis and pericarditis (15,403) are skewed toward the young, average age 32, and toward boys more than girls.

When adults do have myocarditis following the jab, it is equally likely to be after the first or second dose. But when young people (<20) get myocarditis, it is most likely to be after the second dose. My interpretation: Adults have been around the block, and they have seen spike proteins before. Their response to the vaccine is from memory B cells. Young people are more likely to be responding from naïve B cells. Something terrible (that I don’t claim to explain) happens when they see the same antigen 3 weeks later.

Neurological damage, including Bell’s Palsy, paralysis, and Guillain-Barre, peak in middle ages (average age 50)
Middle-aged people are also more likely than the young or old to have anaphylactic responses to the vaccines (8,301 total cases). This is surprising, not only in light of the elevated inflammatory response in older people, but also because the old are more likely to have a problem from original sin.

OVS?
A related phenomenon might be called original vaccination sin. It is peculiar to the newer, cheaper crop of vaccines that are based on a single protein extracted from the virus, rather than on a weakened whole virus, which had been the basis of classic vaccines.
When we develop a vaccine for a pandemic virus based on one small subset of the viral genome, quite predictably, the virus squirm its way out of this artificial barrier by mutating exactly that part of its genome that the vaccine targets. The new variant, with mutations in just the target part of its genome, expands in just a few months from a rare sub-species to become the dominant infection.
Meanwhile, the pharmaceutical manufacturers are geared up to mass-produce a vaccine that no longer targets the current version of the virus. A seasoned Dutch vaccine specialist predicted back in April that just this would happen. As the omicron variant emerges with 37 mutations in the spike protein, scientists who certainly know better feign surprise that so many mutations could arise so quickly, and in just the part of the virus that vaccinated individuals respond to. A high school student’s understanding of natural selection makes it obvious why the COVID virus is mutating in this way.
The good news is that these mutations are likely to make the virus less deadly. The spike protein of SARS-CoV-2 is not an ordinary, evolved spike protein which is evolved to bind well to a receptor and gain entrance to a host cell. This spike protein was engineered in a bioweapons lab to be toxic in multiple ways (in addition, of course, to binding to ACE-2), to break off and enter the bloodstream, spreading its damage far and wide. So when the spike protein mutates to avoid the vaccine, it is likely to become less toxic (while retaining the ability to bind to ACE-2, because that’s what helps the virus to transmit itself.)
OAS and ADE
ADE = antibody-dependent enhancement (or pathogenic priming) is much better known these days than OAS. ADE or PP refers to any situation in which having been exposed to a virus or bacterium once, the patient becomes sicker on the second exposure. It is much discussed now because of the fear that vaccines could induce ADE, so that some vaccinated people might have worse cases of COVID than if they had not been vaccinated. And indeed there is some evidence for this.
There is no agreement in the community about why ADE happens in some patients some of the time, and there is not even good agreement about how to define ADE. It is possible that the antibody binding to the virus can actually enhance its ability to infect, rather than marking it for destruction.
Some of the definitions of ADE are broad enough to encompass OAS. For example, here is a definition from AAAS. Derek Lowe describes ADE:
Dengue fever is a classic example, because it infects humans through four distinct serotypes. If you are infected with one of these and raise a successful immune response, you may well be at increased risk of serious infection with one of the other serotypes. The neutralizing antibodies for one of the types are often not neutralizing for the others, but instead allow that cell-antibody-receptor mechanism to kick in (easier infection of human monocytes), known as “extrinsic ADE”. There’s also an “intrinsic ADE” seen with dengue, which leads to greater viral replication inside infected monocyte cells before they burst and release their contents. The mechanisms for that are still being worked out, but seem to involve suppression of cytokine pathways.
Here is how Eric Brown describes OAS:
Memory B cells producing antibodies of high affinity and specificity established following a primary exposure to one subset of antigens can prevent or significantly dampen responses by naive B cells to new antigens if they are part of a profile that includes antigens present during the primary exposure (5, 6). This is not a problem if the memory response produces neutralizing antibodies to antigens associated with the secondary exposure; however, problems do arise if memory B cells produce nonneutralizing antibodies to the antigens shared between primary and secondary exposures as reported recently in humans exposed to related human coronaviruses (hCoVs) and later infected with SARS-CoV-2 (7, 8). In such a scenario, not only can the memory response be ineffective, it can significantly attenuate the response of newly activated B cells that could have responded effectively to new antigens absent from the original priming event.
The bottom line
.
Our immune systems are more complex than we understand. They
are brilliantly effective most of the time, but respond to novel stimuli
in ways we can’t predict. In general, it seems true that educating the
immune system about a pathogen in advance adds protection when that
pathogen is encountered later. But there are known and unknown
mechanisms by which previous exposure can make a new infection worse.
Vaccine development is an experimental science. The immune system is modified in permanent ways, and there is no theory to tell us whether the benefits or the detriments of an intervention will play out over the years. There is no substitute for long-term trials.
I’ll save the best news for last
The Delta variant had significantly lower mortality than the Wuhan original SARS-CoV-2. Omicron is the up-and-coming strain of COVID, and it has a dramatically lower mortality. There is a simple explanation for this direction of evolution, and I think it’s something we can count on.
In general, viruses evolve to become more contagious and less harmful. It’s in the virus’s interest to co-exist with the host, doing no harm, so it can spread freely. In the case of COVID-19, this evolution has been more rapid and more dramatic than usual. Here’t why:
The spike protein is the part of the virus that is engineered as a bioweapon. The spike protein is responsible for damage to arteries, to nerves, and to the heart that make COVID a fearsome disease. But the spike protein is also the only part of the virus that is induced by the vaccines. Hundreds of millions of people have immunity to the spike protein and nothing else. The virus can continue to spread to the extent that it evades vaccine immunity, and the best way to evade vaccine immunity is via mutations to the spike protein. [recent survey from the SF bay area] These mutations tend to de-fang the spike protein, which was engineered by humans to have multiple toxic effects.
The vaccines are doing their job by guiding the evolution of the virus toward a more benign form. The end game will be that those of us who have not already lived through COVID will be exposed to omicron or something even more benign, and we’ll come through with a lifetime of immunity to all new COVID strains.


No comments:
Post a Comment