What If Cancer Was Already Cured?
How To Activate An Army Of Macrophages To Boost Immunity
By Bill Sardi
December 22, 2021
Looking back, it appears the first realization that cancer had been cured occurred in 2008 when the world learned via this author that white blood cells known as macrophages could be activated to effect a cure. What happened in the aftermath is the subject of this report.
Background: abject failure to cure cancer
False claims of cancer cures are not being made by health quacks but by degreed doctors and “ethical” medical institutions. Cancer care is a business and any dent in the volume of care (1.7 million diagnosed/year) would financially threaten a $175 billion industry. Modern medicine can’t afford to cure cancer says a striking report entitled The Cancer Industry: Hype vs. Reality (Scientific American).
The cancer industry has reached a dead-end (no pun intended). The median cost for new cancer drugs is now above $150,000; the cost of a year of life gained $200,000; the estimated cost to eliminate cancer is $316,641 and would increase total healthcare expenditures 3-fold, thus bankrupting all healthcare
programs. 1 in 3 cancer patients must turn to friends or family to pay for care. Possibly reallocation of funds toward cancer prevention would spare health plans from insolvency, but the problem is that many cancers are not detected until it is too late.Of current interest, ~6% of Covid-19 patients have developed cancer, 1.8-fold greater than those without cancer. Immunotherapy would address both diseases.
Horrible track record for cancer care
- The lifetime risk for cancer is ~40% in humans but just 4% in most all other large-bodied species of animals.
- The 2-year survival of newly diagnosed cancer patients is just 7% over the past 27 years of the War On Cancer.
- Chemotherapy kills cancer patients before their disease does.
- 70% of tumors are solid masses that chemo and radiation cannot penetrate. The treatment failure rate for solid tumors is ~90%.
- Tumor-drug resistance sets in 100% of the time.
- Chemotherapy achieves in 5-year survival only 2% of the time.
- The mortality rate for all cancer in the US, ~152.4 deaths per 100,000 people, hasn’t budged since 1930. In recent decades, the cancer mortality rate has continued to rise.
- Most people who die of cancer exhibit symptomless spread (metastasis) throughout their body. Therefore, the only chance for a cure or prolonged survival is systemic therapy rather than targeted localized treatment.
The cause of cancer remains a confusion, with the statement cancer is 200 different diseases. Yes, but its cure lies within the body, not in some new monoclonal antibody or tricked-out treatment that costs hundreds of thousands of dollars.
Immunotherapy therapy
In 1962 Dr. Chester Southam injected millions of cancer cells into elderly patients to prove the human immune system is capable of resisting cancer even when attempts are made to intentionally induce malignancy.
The re-introduction of macrophage therapy
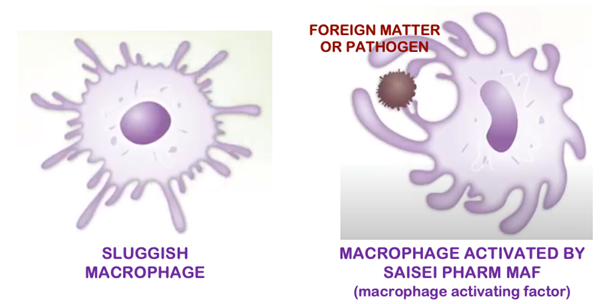
The question of whether modern medicine will ever move away from its treatment-centered approach of disease care towards a curative paradigm is now being tested with the introduction of macrophage therapy. Macrophages (mack-row-fay-jes) are the paramount governors of the human immune system. Macrophages often remain dormant and sluggish as tumor cells and viruses dull the immune response. In the past researchers demonstrated how to activate macrophages, but modern medicine shunned that discovery. If unguided cancer patients want to pursue this macrophage “cure” they have to opt out of the disease-care system.
Once before modern medicine attempted to invigorate macrophages via a monoclonal antibody (a laboratory- produced molecule that substitutes for natural antibodies), but side effects, elevated costs and treatment resistance problems caused this widely heralded treatment to fizzle.
Dr. Yamamoto’s nagalase theory of cancer
From 1990 to 2011 a noted researcher, Nobuto Yamamoto, operating out of what he called The Socrates Institute in his home in Philadelphia, and who is now in his 90s, published ground-breaking human studies to demonstrate that nagalase, an enzyme secreted by viruses and tumor cells, degrades macrophage activating factor (MAF), essentially disarming the large army of reserve macrophages that would normally engulf and kill viruses and tumor cells.
Dr. Yamamoto published four papers that revealed MAF therapy cured colon, breast, prostate and lung cancer in humans with remissions lasting 4-7 years when subjects were administered just 100 billionths of a gram of MAF. Similar studies produced the same result. Yamamoto’s monumental achievement was ignored. This author along with laboratory scientist and tipster Timothy Hubbell broke this story in 2008 to the public at large.
Modern medicine wasn’t ready to accept Dr. Yamamoto’s definition of a cure, which was to administer macrophage activating factor (MAF), a derivative of vitamin D-binding (transport) protein, and measure its effectiveness by charting nagalase enzyme levels, thus effecting a cure. But alleged deficiencies in his research papers resulted in his work being discredited. Some of his published papers were retracted. Such is the fate of anyone who cures cancer. We have reached a point where any cure for cancer is a threat to a $175 billion industry.
Is modern medicine finally going to put macrophage therapy to the test?
Fast forward—a recently published report entitled “Targeting macrophages in cancer immunotherapy,” suggests modern medicine may turn its cannons around and begin learning how to use macrophage therapy for otherwise unconquerable maladies. But we’ve been down this road before.
That report concedes that there are limitations of traditional cancer treatments, the slash, burn and poison approach to cancer has failed, and immunotherapy has become the most promising cancer treatment.
Furthermore, it’s not like macrophage therapy has been completely abandoned. There are over 150 human clinical trials, some withdrawn, some terminated, that involved macrophage-targeting agents. A report says: “Macrophages provide a force to be considered in immunotherapy and might be a new door for oncotherapy.”
In 2017 researchers lamented over the fact MAF therapy has been successfully demonstrated; that the nagalase enzyme that disarms macrophages is not detected in healthy individuals; that MAF increases cell counts of macrophages by 40-fold; and questioned why MAF therapy has not been approved by health authorities; and suggested non-scientific reasons for ignoring its potential. In other words, cancer has been cured, but the cure has been swept under the rug.
Modern immunotherapy flops
Drug firms aggressively market immune therapies “even when there is little to no evidence these drugs will work,” says a report in Scientific American. Fewer than 10% of cancer patients benefit from conventional immune therapies. If widely prescribed, they would bankrupt the American health-care system.
A widely heralded type of immunotherapy for cancer called CAR-T-cell therapy involves removal, activation and re-instillation of T-cells to attack cancer cells. A recent report concedes that while CAR-T-cell immunotherapy has been widely hailed for its ability to quell blood cancers, it has been a disappointment for solid tumors. For that reason, macrophage therapy is now being considered.
Another advantage of macrophage activation is that it does not induce tumor cell resistance as does chemotherapy.
Will it happen this time?
We now read reports in the medical literature with titles like “Macrophages Hold The Key To Cancer’s Inner Sanctum,” and “Is Nagalase The Key To Curing Cancer?”
Researchers go on to say macrophage activating factor (MAF) is so essential to producing immunity that it should even be used as an adjuvant (additive) to all immunizations.
Nagalase
Nagalase’s ability to degrade MAF is so critical that its inhibition has been called “the key to curing cancer.”
Nagalase is also attributed to the pathogenicity of some viruses.
A high level of nagalase activity is related to tumor growth and loss of infection control.
The macrophage paralyzing nagalase enzyme is ~10 times greater in cancer patients versus healthy patients. It was only recently (2017) that researchers in the Netherlands confirmed that nagalase, which escaped detection in earlier studies, is in fact in high concentrations in cancer patients and researchers said this now confirms Yamamoto’s earlier work.
Overlooked study: nagalase enables influenza
An overlooked study published in 2005 showed that nagalase is the intrinsic component of hemagglutinin, a glycoprotein (sugar/protein) found on the surface of influenza viruses that facilitates viral binding (infection) to cells in the human body. Modern medicine has been keeping nagalase research in the closet for too long a time.
Of interest, the trace mineral zinc inhibits nagalase.
History and scientific background
Macrophages were first discovered by Elie Metchnikoff, a Russian zoologist, in 1884.
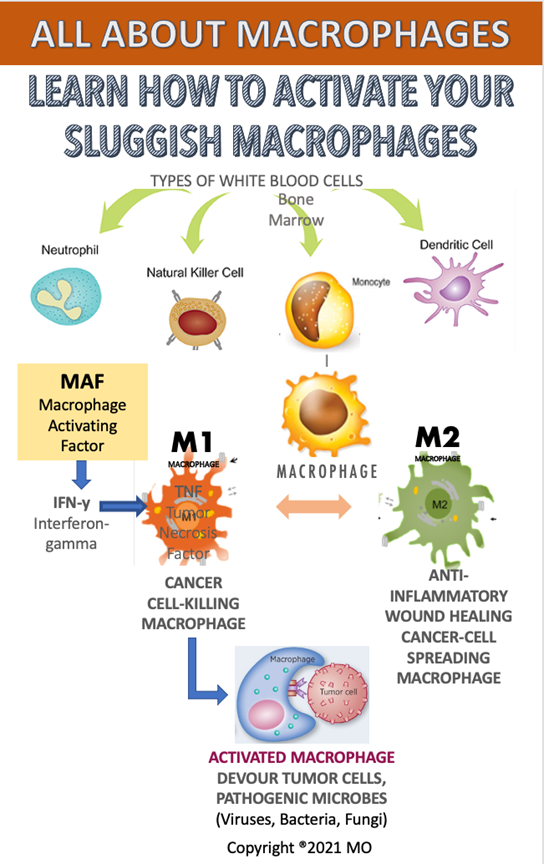
Derived from white blood cells called monocytes, an army of ~200 billion microbe-devouring macrophages (mack-row-fay-jes), with a lifespan ranging from months to years, continually surveil your body for pathogenic bacteria, viruses, fungi, and mop up heavy metals such as iron, and tumor cells.
Macrophages are known as the janitors of the human body, clearing out dead cells and cellular debris. Every day about 200 billion red blood cells die off and macrophages engulf and dispose of them. In that clean-up process macrophages recycle almost 3 kilograms (over 6 lbs.) of iron and hemoglobin each year to reuse.
While lysosomes clean inside cells, macrophages devour and remove debris from the connective tissue between cells. This clearance process is vital without which humans could not live.
As sentinels of harmful threats, macrophages comprise ~10% of the total white blood cells in your body, they go by different names in different tissues and organs: osteoclast (bone); glia (brain); Kupffer cells (liver); retinal pigment epithelium (retina); Langerhans cells (skin). These are stagnant phagocytic (devouring) cells in their respective tissues. It is the reserve supply of phagocytes that roam the body and remove foreign material.
Roaming macrophages derived from monocytes, another class of white blood cells, are classically identified as M1 (highly inflammatory, tumor killing) and M2 (anti-inflammatory, tumor promoting). They are very plastic (inter-changeable) cells that cannot be easily stereotyped.
Recently researchers experimentally used a laser to split a blood vessel in two and then watched miraculously as macrophages literally seized the broken ends of the blood vessel and stuck them back together. Click and watch this.
Macrophages can extend arms from its body to surround and engulf a dangerous microbe or tumor cell. In fact, macrophage comes from the Greek words Macro meaning “large” and Phage meaning “to eat.” The process of engulfing and killing foreign substances is called phagocytosis.
Where macrophages come from
Macrophages In Action
Bone marrow produces white blood cells called monocytes that then morph into macrophages. There is more than one way to activate macrophages. T-cells (thymus gland-generated cells) may trigger macrophages. Interferons and tumor necrosis stimulate macrophages. When macrophages are overactive, they can ignite inflammation.
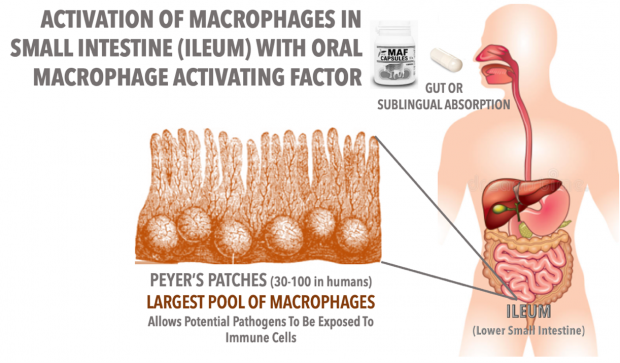
The largest pool of macrophages is present in Peyer’s Patches (named after Swiss pathologist Johann Conrad Peyer who first described them in 1677), seen as small bumps in the distant end of the small intestine (ileum). It is this reserve horde of sometimes-idle macrophages that can be paralyzed by nagalase but also can be directly stimulated by an oral or injected activator like MAF in the digestive tract.
Iron and macrophages
In 1959 researchers first showed that iron injected into muscle to induce malignant tumors. Iron chelators (binders) have been successfully demonstrated to combat cancer.
Excess iron inhibits the tumoricidal/virucidal/bactericidal activity of macrophages. Increased iron and copper concentration in macrophages reduces their activation by interferon. Though tumor-associated macrophages can be heated (hyperthermia) to release superparamagnetic iron oxide to kill cancer cells. This approach is being explored.
Iron accumulates in the body after full childhood growth is achieved, first in males and later in females as monthly menstrual blood losses cease with menopause. Iron overload explains why cancer is a disease of aging and why older adults are more prone to infections.
Iron is stored in a binding protein called ferritin, which is where bone marrow gets iron to make new red blood cells. The Iron Disorders Institute considers a ferritin level of 25-75 nanograms per milliliter blood sample as a healthy range, but ferritin levels in reach 1000 ng! Given that 90% of iron is housed in red blood cells, blood-letting (phlebotomy) is called for at this point. Excessive iron stores can paralyze macrophages!
Iron and copper are used by bacteria and tumor cells for growth and iron/copper overload impairs the phagocytic action of macrophages. By virtue of macrophages mopping up loose unbound iron, tumor-associated macrophages will either withhold iron to stunt tumor growth or actually deliver iron to tumor cells to oxidize (kill) them. Macrophages being highly adaptive, iron in macrophages can also activate killing of bacteria and tumor cells.
Alcohol + iron = nagalase
Of interest is that alcohol consumption increases iron absorption from foods and alcohol is also associated with increased nagalase enzyme activity.
Over two drinks of alcohol per day dramatically increases iron absorption, especially when consumed with food. It is no surprise to learn that iron overload increases risk for liver cancer by 20-200 times and lung cancer by 3-fold.
Iron removal quells growth of tumors and microbes and activates macrophages. Iron-containing enzymes are required for viruses to replicate. Iron/copper chelators would be advantageous in the control of malignancy. In lieu of blood/iron removal (blood letting), or inositol hexaphosphate (IP6, Tsuno Foods, Wakayama, Japan), the natural metal-chelator extracted from rice bran, can be consumed to remove loose iron and has a profound effect on macrophages.
Companion treatment
Of additional interest is that macrophage activating factor (MAF) is derived from vitamin D binding protein and the combination of vitamin D + IP6 rice bran dramatically increases IP6 utilization.
Investigators now realize the internal production of interferon cannot sustain a population of activated macrophages. Other immune cells (T-cells) help to activate macrophages of out dormancy. This is where macrophage activating factor (MAF) comes in. In states of disease or infection macrophages are predominantly activated by vitamin D-binding protein/macrophage activating factor (MAF).
MAF Therapy: Japan
Researchers at the Saisei Mirai clinics in Japan, led by Dr. Toshio Inui, combined with investigators at Tokushima University, then picked up the ball and in 2013 began clinical use of MAF for cancer patients. It was reported 345 consecutive end-stage cancer patients were successfully treated (experienced extension of survival) with MAF + vitamin D therapy.
Using a 2nd generation MAF, in 2013 the Saisei Mirai Clinic MAF combined treatment regimen is reported to have turned macrophages into natural killer cells.
There are a number of MAF products sold online, some for topical application, which would be a specious value. The primary health benefit arises from activation of the reserve pool of macrophages in the distal small intestine (ileum; in Peyer’s patches). Saisei Pharm MAF is now used in 8 clinics in Japan and worldwide.
Indirect attempt to block nagalase with a decoy molecule
As an alternative to MAF, a commercial venture was launched utilizing chondroitin sulfate as a decoy molecule to block the binding of nagalase to MAF/vitamin D-binding protein. Chondroitin sulfate is widely available and is complexed with oleic acid (olive oil) to enhance absorption in an over-priced dietary supplement. A vitamin D/MAF derived from fermented milk, fish oil and aspirin combination is reported to reduce tumor size by 25%.
Venturing forward
In what is the boldest advancement thus far, MAF researchers at Saisei Pharma in Japan serve as sponsor for a study using Saisei Pharm MAF for coronavirus infection. The studies are listed at ClinicalTrials.gov.
The US FDA recommended a small proof-of-concept study before launch of a 600-patient MAF (Saisei Cov UKRAINE) study among hospitalized subjects.
The results of that preliminary study of hospitalized COVID-19 patients revealed mortality of 4 of 16 patients receiving an inactive placebo and 0 of 16 patients receiving Saisei Pharm MAF oral capsules. NO adverse events were reported.
A second Phase 2 study is also underway in Italy. In fact, as of December 2021 these two studies have now been completed and results may soon be reported, and could turn the infectious disease world upside down.
Oral MAF capsules available in US
 A 3rd-generation
encapsulated oral MAF SAISEI PHARM dietary supplement is now available
for use without prescription in the US. This version of SAISEI PHARM
MAF is solely intended to support healthy immunity and macrophage
activity and is not intended for prevention, treatment or cure of any
disease.
A 3rd-generation
encapsulated oral MAF SAISEI PHARM dietary supplement is now available
for use without prescription in the US. This version of SAISEI PHARM
MAF is solely intended to support healthy immunity and macrophage
activity and is not intended for prevention, treatment or cure of any
disease.
It is expensive: $210 for 60 capsules (2-a-day regimen; 30-day supply; telephone 702 682-9945 toll free). It’s intended use is to help infirm individuals regain health. Because of its expense, it is not suggested for continued use to maintain health. It can be used with other medicines and treatments and should be accompanied by 8000 IU of vitamin D3 per day. Saisei Pharm MAF capsules are shelf stable at room temperature and have a shelf-life of ~3 years. (Note: This product is not the same being used in the human clinical study for Covid-19.)
What do you do now?
Questions whether macrophage activation pertains to certain types of tumors are immaterial. Macrophages pay no heed to the location of cancer, the type of cancer, the size of the tumor(s), or the stage of cancer?
Why should any cancer patient go to their deathbed with low vitamin C and D levels, excessive iron levels and sluggish macrophages? No double-blind, placebo-controlled study needs to be performed to prove MAF activates macrophages. A healthy body produces MAF. There are no significant side effects associated with MAF therapy.
MACROPHAGES may be quiescent or idle, waiting to be activated by MAF in states of infection or malignancy. Or macrophage activator (MAF) may be degraded by nagalase, and nagalase needs to be inhibited.
Viruses and tumor cells rampantly divide and overwhelm tissues and organs because they degrade MACROPHAGE ACTIVATING FACTOR via the enzyme NAGALASE. At this point of desperation, MACROPHAGE ACTIVATING FACTOR (MAF) itself must be direcetly administered.
Modern medicine has its own forms of immunotherapy, and they cost hundreds of thousands of dollars. The regimen described herein gives sick patients a chance to affordably optimize their immune system.
What would this author do if diagnosed with cancer?
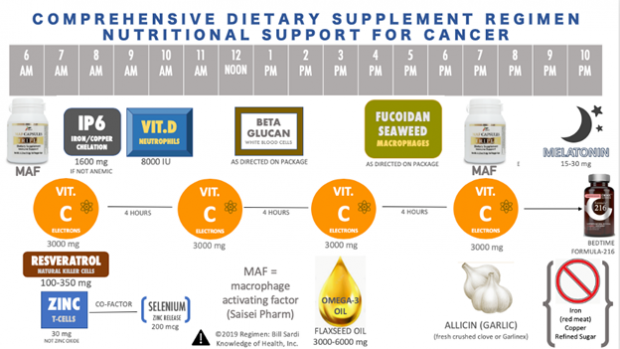
If I was diagnosed with cancer today I would embark on a MAF regimen, 2 capsules per day. I would add vitamin D3 (at least 8000 IU per day) and vitamin A 2500-5000 units/day to normalize the immune response; and 30 mg of zinc to activate vitamin D to its active form (calcitriol) and to reduce nagalase; and 200 micrograms of selenium to release zinc; and take an iron chelating dose of rice bran IP6 (800-1600 mg) per day for 30-90 days; and 100-250 milligrams of the red wine molecule resveratrol to sensitize vitamin D’s entry into cells and to inhibit growth of new blood vessels that feed solid tumors.
Additionally, chondroitin sulfate 500 mg could be taken to block binding of nagalase to vitamin D-binding protein.
Normalizing macrophages
It is important to control the immune response to pathogens. Both vitamin A and vitamin D inhibit inflammation caused by overactive macrophages to the point of normalcy. Vitamin D contributes to the germ-fighting capabilities of macrophages. 2500-5000 IU vitamin A is a standard dose.
Vitamin C
Macrophages contain 10-40 times more vitamin C than blood plasma. Vitamin C has been demonstrated to reduce oxidation in activated macrophages. Vitamin C has been shown to increase cancer-cell-killing of macrophages by 40% via its ability to increase nitric oxide gas. Activated macrophages use vitamin C to limit oxidation caused by macrophages themselves.
Suggested regimen: Vitamin C, 3000-4000 mg every 4-6 hours and/or a novel vitamin C supplement that doubles vitamin C levels by internal synthesis (Formula-216). The internal conversion of blood sugar, which feeds cancer growth, to ascorbate (vitamin C) would deprive tumors of the sugar they use for growth. Intravenous vitamin C is also suggested.
All these dietary supplements are intended to optimize immunity, and no claim is made that any of these products individually or collectively cure, treat or prevent cancer. Given that there is NO CURE for cancer, is there any harm in trying if there are no side effects?
Truthful information about dietary supplements
A recent Supreme Court Ruling states “truthful promotion” of off-label uses of drugs is Constitutionally protected speech beyond the regulatory reach of the FDA. Any ban on distribution of truthful information that would interfere with the ability of consumers and physicians making intelligent decisions, should be outside of the purview of the FDA. It’s truthful to say MAF activates sluggish macrophages, and zinc inhibits nagalase, the enzyme that degrades MAF.
Case presentation
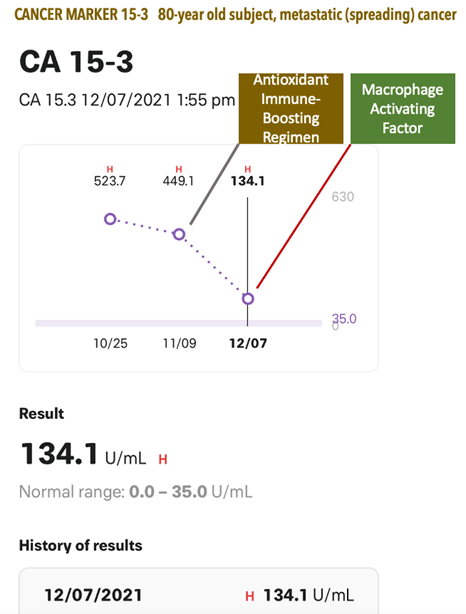
The effectiveness of MAF therapy is evidenced in a case of metastatic cancer in an 80-year-old subject with a CA 15-3 who first used antioxidants, trace minerals and polyphenols to reduce the tumor marker from 523.7 to 449.1. Then a month of MAF therapy dramatically reduced this tumor marker to 134.1 (normal range is below 30; see below).

No comments:
Post a Comment