Hypothesis: ultrasonography can document dynamic in vivo rouleaux formation due to mobile phone exposure
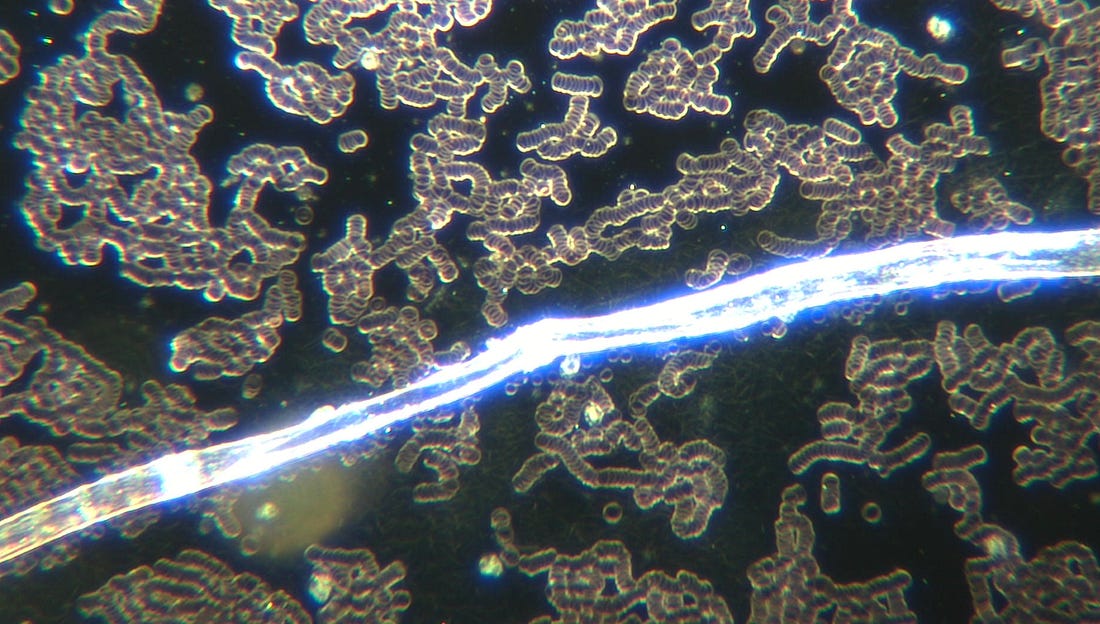
This
case report shows rouleaux formation in a leg vein after cell phone
exposure via ultrasound. Live blood analysis is also a great way to show
immediate rouleaux formation with exposure to smart phones. It also
enhances the growth of the filaments and microchips in the blood -
ultimately these blood changes increase the risk of blood clots and
diminish oxygen delivery capacity of the red blood cells.
Image: COVID19 unvaccinated blood with polymer contamination after holding a cell phone. Magnification 200x. AM Medical.
Abstract:
Carrying
a cellphone against the body has become commonplace in our world
replete with smartphones. Acute and chronic health effects caused by
these devices emitting radiofrequency radiation from multiple antennas
have not been well evaluated. In this study, the popliteal vein of a
healthy volunteer was imaged with ultrasonography prior to and following
the placement of an idle, but active smartphone against her knee for
5 min. Pre-exposure longitudinal sonographic
images demonstrate a normal
anechoic lumen to the popliteal vein. Images obtained 5 min after
direct skin exposure to the smartphone demonstrate a dramatic change in
the acoustic appearance of the vessel. The interior of the vessel became
coarsely hypoechoic with sluggish flow seen in real-time images, a
typical sonographic appearance for rouleaux formation. A follow up
examination performed 5 min after the subject walked around yielded
continued rouleaux formation in the popliteal vein, albeit less dramatic
than that observed immediately post exposure. This revolutionary in vivo
method to assess radiofrequency radiation induced rouleaux formation
should be further pursued in the general population to determine its
prevalence and if its occurrence provides a unique biomarker of exposure
that may predict morbidity.
Researchers
have reported red blood cell (RBC) aggregation, referred to as rouleaux
formation, in people who have been recently exposed to electromagnetic
fields and radiofrequency radiation. To date, the static technique of
live blood cell analysis utilizing dark-field microscopy has been the
method of choice to evaluate this phenomenon. Because this in vitro
analysis may be compromised by artifact from imperfect technique, we
sought to produce a novel and innovative approach to this question by
devising a noninvasive, in vivo method for
assessing the presence of rouleaux formation. Diagnostic ultrasound has
been the preferred modality for evaluating the blood flow pattern in
veins for decades. Although studies are often performed to assess for
deep venous thrombosis or venous insufficiency, the presence of rouleaux
formation can be readily observed. We hypothesize that ultrasonography
provides a simple, non-invasive in vivo diagnostic tool to detect the presence of rouleaux formation in individuals following exposure to radiofrequency radiation.
We
performed a series of studies on a 62-year-old asymptomatic healthy
female volunteer with no history of allergy, blood disorder, or systemic
disease. The volunteer is not on any medication and her only remarkable
medical history is having received a pneumococcal vaccine for a lack of
pneumococcal antibodies during the previous year. She had no available
blood work.
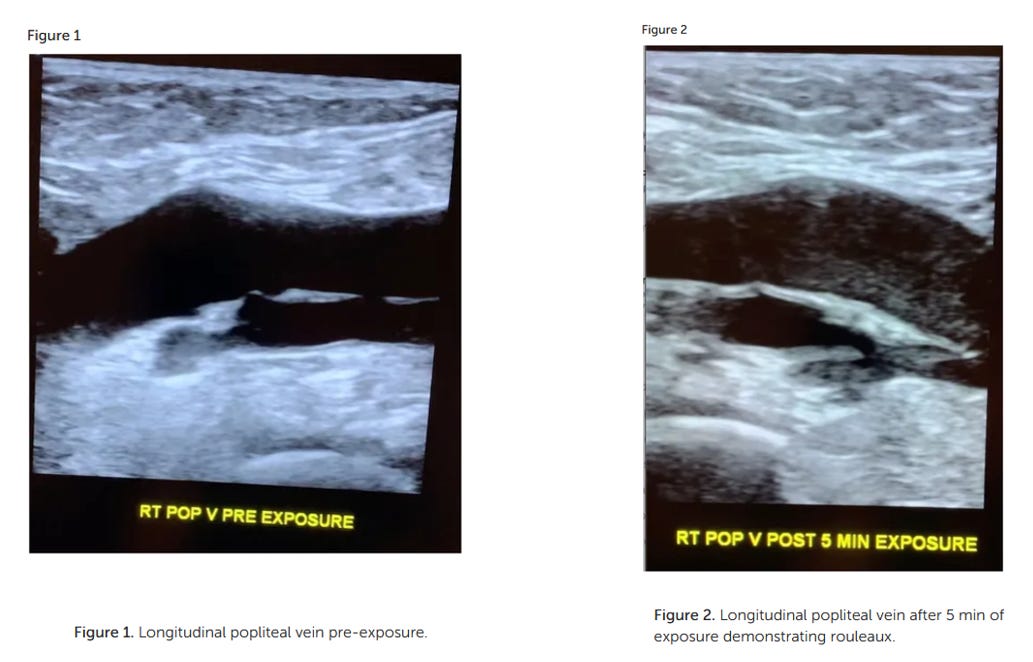
The
subject was placed on a gurney and draped with her leg exposed. A GE
Logic E10 ultrasound machine was utilized with an L2–9 linear probe to
image the popliteal fossa. The machine has auto focus and time-gain
compensation (TGCs) on a touch screen menu, which can be adjusted by the
sonographer to optimize images. A senior ultrasonographer with over 25
years of experience performing vascular ultrasound identified the
popliteal vein and obtained cine longitudinal images to confirm the
vessel lumen was anechoic (Figure 1).
Immediately following, an Apple iPhone XR smartphone operating on the
AT&T mobile network was placed on the popliteal fossa for 5 min. The
phone's Wi-Fi, Bluetooth, and cellular data antennas were all turned
on, but the phone was otherwise inactive and idle. No calls or text
messages were received during the 5-min time interval. Note however that
even when a phone is not being used to make a call or send a text,
devices continually update apps that require uploading and downloading
from cellular networks.
Following exposure, the subject's popliteal vein was reimaged (Figure 2).
No changes were made in between the two scans on the ultrasound consol.
Specifically, there was no adjustment to the total gain or TGCs that
could cause a change in apparent echogenicity of the popliteal
structures as compared to pre-exposure images. A post exposure cine loop
demonstrates abnormal heterogeneous, predominately hypoechoic material
sluggishly moving to and fro within the popliteal vein and nearby
tributaries. The sonographic appearance is typical for rouleaux
formation, named for the histologic appearance of red blood cells when
they are stacked upon one another, resembling a stack of coins. The
subject experienced no symptoms.
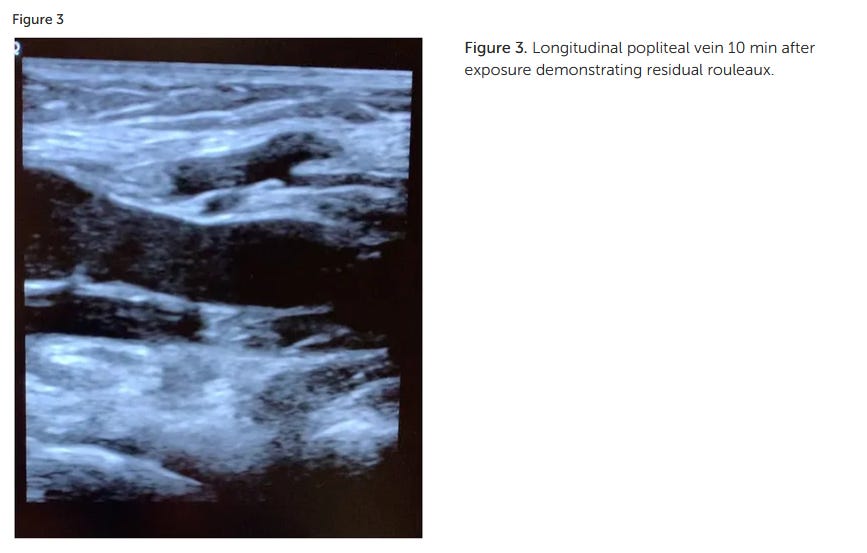
The
subject walked for 5 min after the second scan to see if the rouleaux
formation would dissipate with exercise and then reimaged a 3rd time.
The final imaging cine loop (10 min after exposure) demonstrate
continued rouleaux formation, but the conspicuity of the aggregates had
diminished as compared to the immediate post exposure images (Figure 3).
Two
months after the initial study was performed, the subject returned to
the ultrasound department and was reimaged utilizing the same protocol.
Pre-exposure images demonstrated a normal anechoic lumen in the
popliteal vein. Images obtained 5 min after cell phone exposure to the
popliteal fossa again produced rouleaux formation, confirming
reproducibility of the initial observation.
The
subject returned 6 weeks later for a third and final assessment. During
this imaging session, grey scale and duplex doppler pre-exposure images
of the right and left popliteal vein were taken with the subject supine
and also while standing. The pre-exposure images demonstrated a normal
anechoic lumen to the popliteal veins in both lower extremities. An
Apple iPhone 16 plus was then placed against the right popliteal fossa
for 5 min. Following, images of the right and left popliteal veins were
then obtained with the subject supine and standing. Post exposure images
demonstrate rouleaux formation in both lower extremities.
I
am also attaching this recent email from Professor Olle Johannson
regarding the updated safe screen times for children. Please see our eye
opening interview here where he explains that none of the EMF devices
for cell phones work.
The
Dangers of EMF Radiation - Conversation With World Expert In EMF
Radiation Professor Dr. Olle Johansson - Truth, Science and Spirit:
Episode 20
The enclosed very important press release from The Spanish Association of Paediatrics (AEP)
is not primarily about the exposure issues to man-made electromagnetic
fields, but on the use of screens in childhood and adolescence.
However,
as such it can be used as a strong lever to introduce also discussions
about adverse health and biological effects of these synthetic
electromagnetic fields, such as from cell phone systems, WiFi, tablets,
laptops, high-frequency light bulbs, wireless smart meters, baby alarms,
DECT phones, powerlines, smart cities, the Internet of Things and the
Internet of Bodies, 5G, 6G, 7G, and much more. They are to be viewed as a
non-evolutionary-adapted form of radiation, and may therefore be
labeled 'potentially toxic to life on the planet' [cf. Johansson O, "The
Stockholm Declaration about "Life EMC"", Bee Culture Magazine 2022; May
issue: 56-61 --- Johansson O, "Our bacteria: are they trying to tell us
something?”, Newsvoice.se 20/6, 2022 --- Johansson O, "Stop! In the
Name of Life!”, Newsvoice.se 9/1, 2025].
Here is the press release:
The Spanish Association of Paediatrics (AEP) updates its recommendations on the use of screens in childhood and adolescence.
Published on 05-12-2024
https://www.aeped.es/noticias/aep-actualiza-sus-recomendaciones-sobre-uso-pantallas-en-infancia-y-adolescencia
Madrid,
5 December 2024 - The age range below which it is considered that
children should not be exposed to screens has increased from 2 to 6
years of age.
A strong association is shown between
parents' screen time and their children's screen time, especially at
mealtimes and in the bedroom.
It is corroborated that
the excessive use of screens harms areas such as sleep, cardiovascular
risk, brain volume and nutrition, among others.
The
Spanish Association of Paediatrics urges governments and the education
system to take measures to avoid the potentially harmful effects on the
health and development of children and adolescents.
With
the aim of learning to use technologies in a positive way and reducing
the risks involved in their inappropriate use, the Spanish Paediatrics
Association (AEP), through the Digital Health working group of the
Health Promotion Committee, launched the AEP's Family Digital Plan in
2023, a guide of recommendations adapted to the needs of each family and
the age of the minors in it. It also drew up another document of
suggestions entitled ‘Impact of digital devices on education’, which
complemented the Plan. The commitment adopted by this working group was
to review the content annually according to the scientific evidence
accumulated over the last year. Thus, following this analysis, the new
recommendations will soon be published in an article in Anales de
Pediatría, the AEP's scientific journal, and on the Family Digital Plan
website itself.
‘Nowadays no one doubts that digital media affect health at all levels, and at any age,’ explains Dr María Salmerón, coordinator of the AEP's Digital Health working group. ‘In
2016, the American Academy of Paediatrics warned for the first time of
the impact of the digital world on health, and in recent years there has
been a progressive increase in clinical trials that corroborate this
link’, adds the expert.
The
impact of excessive screen use in childhood and adolescence is
multifactorial, affecting various areas related to health and
well-being, reducing quality of life.
More information in the attached press release.
https://www.aeped.es/sites/default/files/20241205_ndp_aep_actualizacion_plan_digital_familiar_def.pdf [NdP_update_plan_digital_familiar_plan.pdfthe children's declaration]
'All this scientific evidence has led us to update the age-specific recommendations on the use of screens’, explains Salmerón.
0 to 6 years:
● Zero screens, there is no safe time.
● As an exception and under adult supervision, they can be used for social contact with a specific
specific objective. For example, the person on the other side of the screen can tell a story or sing a song.
a story or sing a song.
7 to 12 years:
Less than one hour (including school time and homework).
● Limit use of devices with Internet access.
● Prioritise protective factors: sporting activities, face-to-face peer relations,
contact with nature, sleep, healthy eating, etc.
●
If it is decided that they should use a device, it is recommended that
it be under the supervision of an adult, with fixed devices, and that
●
If it is decided that they should use a device, it is advisable: under
adult supervision, with fixed devices and avoiding the bathroom and
bedroom.
● Agree clear limits beforehand, both in terms of time and content adapted to age.
13 to 16 years:
Less than two hours (including school time and homework).
● If access to devices is allowed - but not the only measure to be taken - install parental control tools.
Olle Johansson, associate professor
No comments:
Post a Comment