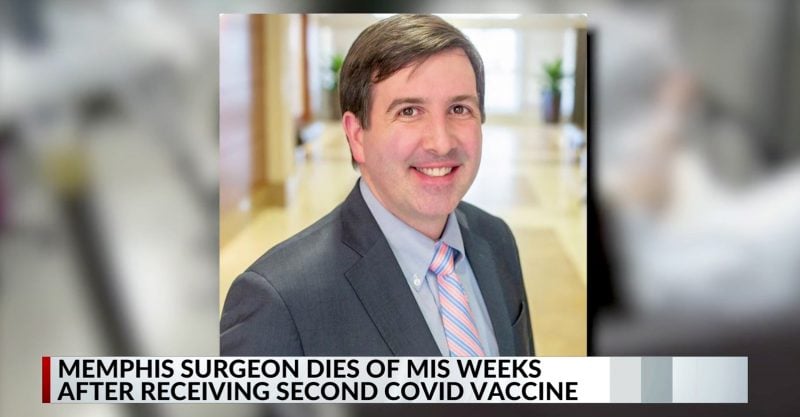
36-Year-Old Doctor Dies After Second Dose of COVID Vaccine
News reports attributed Dr. Barton Williams’ death to multisystem inflammatory syndrome (MIS-A) caused by asymptomatic COVID, though he never tested positive for the virus.
The Centers for Disease Control and Prevention (CDC) is investigating the death of a 36-year-old doctor in Tennessee who died Feb. 8, about a month after receiving the second dose of a COVID vaccination.
According to news reports, Dr. Barton Williams died from the adult form of multisystem inflammatory syndrome (MIS-A), a condition caused when the immune system attacks the body resulting in multi-system organ failure. MIS-A is considered extremely rare.
The Daily Memphian and other news sources reported that those involved in the investigation believe
Williams developed MIS-A in response to an asymptomatic case of COVID-19, not the vaccine.Dr. Stephen Threlkeld, an infectious disease specialist who treated Williams and is working with the CDC to investigate the death, told a Memphis ABC News affiliate that Williams tested negative for COVID while in the hospital and that Williams had told him that to his knowledge, he had not the virus.
However, Threlkeld said testing revealed “two types of antibodies in [Williams’] system — one type of antibody that results from a natural COVID infection, and a second type of antibody from the vaccine.”
Asked whether the vaccine, rather than an asymptomatic case of COVID, could have caused Williams to develop MIS-A, Threlkeld said: “Everyone who has had [MIS-A], has had the infection. There has been no case published yet of someone who has been documented to have this problem, who has been vaccinated in the past.”
Threlkeld also said: “This is not a reason, not to get the vaccine. It’s a reason to get the vaccine, because only people who have had the infection have had this occur.”
But Lyn Redwood, RN, MSN, president emerita of Children’s Health Defense questioned the preliminary findings that ruled out the vaccine in favor of a rare reaction to an asymptomatic case of COVID.
Redwood pointed to research that described temporal associations between Kawasaki disease (KD), a disease that exhibits symptoms similar to MIS-C such as high fevers, rash and blood vessel inflammation, and a wide variety of vaccines, including hepatitis A and B, rotavirus, influenza, DPT or DTaP, pneumococcal vaccines and yellow fever.
“Scientists who have studied the “distinctive immune system characteristics” of children with Kawasaki disease, a disease which is very similar to MIS-C, acknowledge that the ‘antigenic stimulation’ set in motion by vaccines and other biologics has the capacity to create “immunologic interference,” Redwood said. “Is it possible that the MIS-C and MIS-A are the result of ‘pathogen priming,’ a mechanism that other researchers euphemistically describe as ‘immune enhancement’?”
“Pathogen priming can arise when the proteins in viral vaccines are so similar (‘homologous’) to proteins in humans that they subsequently trigger out-of-control autoimmunity or hypersensitivity reactions such as shock syndrome and delayed anaphylaxis,” Redwood said.
As Redwood reported earlier this week, research has found the SARS-CoV-2 spike protein alone — without the virus — to be a potent inductor of endothelial dysfunction, suggesting that “manifestations of COVID-19 shock syndrome in children can be at least partially attributed to its action.”
MIS-C, the childhood version of multisystem inflammatory syndrome, is also rare, but more common in children than adults. Children with MIS-C often exhibit symptoms similar to Kawasaki disease.
In her Feb. 10 article, Redwood referred to a public comment submitted in December to the U.S. Food and Drug Administration from Dr. J. Patrick Whelan, a pediatric rheumatologist, warning about the potential for mRNA vaccines designed to create immunity to the SARS-CoV-2 spike protein to instead cause injuries.
Both the Pfizer and Moderna vaccines, the only two so far approved for emergency use in the U.S., use mRNA technology.
Whelan’s training (at Harvard, Texas Children’s Hospital and Baylor College of Medicine) includes degrees in biochemistry, medicine and rheumatology. For 20 years, he worked as a pediatric rheumatologist. He currently specializes in treating children with multisystem inflammatory syndrome (MIS-C), which has been associated with coronavirus infections.
In his comments to the FDA, Whelan wrote:
“I am concerned about the possibility that the new vaccines aimed at creating immunity against the SARS-CoV-2 spike protein have the potential to cause microvascular injury to the brain, heart, liver and kidneys in a way that does not currently appear to be assessed in safety trials of these potential drugs.”
Whelan was referring to the fact that mRNA vaccines work by incorporating the genetic blueprint for the key spike protein on the virus surface into a formula that — when injected into humans — instructs our own cells to make the spike protein.
In theory, the body then will make antibodies against the spike protein to protect against SARS-CoV-2 infection.
“The problem with this scenario,” said Redwood, “is that the spike protein alone — which the mRNA vaccines instruct the body to make — has been implicated as a key cause of injury and death in COVID-19 infections.”
Based on the research conducted to date, Redwood said, it is very likely that some recipients of the spike protein mRNA vaccines will experience the same symptoms and injuries associated with the virus.
Again according to Whelan, “the potential to cause microvascular injury (inflammation and small blood clots called microthrombi) to the brain, heart, liver and kidney … were not assessed in the safety trials.”
Last year, Canadian researchers identified Kawasaki disease as a “condition of interest” for pediatric vaccine safety surveillance, citing ongoing reports of KD to passive systems monitoring adverse events following immunization (AEFI).
Two studies — one conducted in Singapore and one in the U.S. — have highlighted an association between the 13-valent pneumococcal conjugate vaccine (PCV13) and Kawasaki disease:
- The Singapore researchers looked at all young children (under age two) hospitalized for KD in their hospital from 2010 to 2014, considering children in whom KD onset took place within one month of PCV13 vaccination. Writing in Nature in 2019, the authors denied any overall increased risk but reported “an approximate two fold increased risk of Complete KD within the 28 day risk interval following receipt of the first dose of PCV13.” The researchers closed with an “urgent” plea to confirm their findings.
- The U.S. study, a 2013 Vaccine Safety Datalink analysis by Kaiser Permanente researchers at eight managed care organizations, also looked at children two years and under, comparing those who received PCV13 from 2010-2012 to same-age children who received the Prevnar-7 vaccine (PCV7) in the mid-2000s. For the PCV13-vaccinated infants and toddlers, the likelihood of developing KD was 1.94 times higher than for those who received PCV7 — again representing a finding deserving of “further investigation.”
Sign up for free news and updates from Robert F. Kennedy, Jr. and the Children’s Health Defense. CHD is implementing many strategies, including legal, in an effort to defend the health of our children and obtain justice for those already injured. Your support is essential to CHD’s successful mission.