The Truth About COVID-19 'Long-Haulers'
- November 20, 2020
Story at-a-glance
- 18.1% of individuals diagnosed with COVID-19 also received a first-time psychiatric diagnosis in the 14 to 90 days afterward. Most common were anxiety disorders, insomnia and dementia
- An estimated 10% of patients treated for COVID-19 report fatigue, breathlessness, brain fog and/or chronic pain for three weeks or longer. This phenomenon occurs even among patients who had mild cases of COVID-19
- U.S. Centers for Disease Control and Prevention data show the rate of COVID-19 patients who continue experiencing lingering health problems after recovering from acute COVID-19 may be as high as 45%
- Many post-acute COVID-19 patients fit the diagnostic criteria for ME/CFS, which has been linked to viral infections
- According to a COVID-19 treatment guide, many of these “long COVID” patients do spontaneously recover — albeit slowly — with holistic support, rest, symptomatic treatment and gradual increase in activity
You may have seen reports about COVID-19 patients who seem unable to fully recover. Some complain of lingering chronic fatigue symptoms. Others struggle with mental health problems.
In fact, a study1,2 from Oxford University published online November 9, 2020, in The Lancet Psychiatry, found 18.1% of individuals diagnosed with COVID-19 also received a first-time psychiatric diagnosis in the 14 to 90 days afterward. Most common were anxiety disorders, insomnia and dementia. A similar trend was also observable after COVID-19 relapses.
Interestingly, people with pre-existing mental illness were also found to be 65% more likely to be diagnosed with COVID-19 than those who did not have a pre-existing psychiatric problem.
Now, while this may sound terrifying, I would point out that, given the fearmongering surrounding COVID-19, it's not surprising that receiving a diagnosis would trigger anxiety and insomnia in many. It doesn't mean you end up with a chronic psychiatric disorder. It just tells us that getting a COVID-19 diagnosis is very stressful, even if you remain asymptomatic.
The link to dementia is interesting, however, and likely needs to be looked into further. This also applies to the higher risk of COVID-19 if you have a pre-existing mental health problem. It's possible that people struggling with depression, anxiety and similar disorders are simply more likely to get tested for COVID-19 — and end up receiving false positive diagnoses.
As discussed in "Asymptomatic 'Casedemic' Is a Perpetuation of Needless Fear," mass testing of asymptomatic people doesn't tell us anything of value since the test cannot discern between an active infection and the presence of nonreproductive (harmless) virus. It only makes the pandemic appear graver than it is.
That said, going through a severe bout of COVID-19 is also going to take a mental toll. As reported3 by a 40-year-old previously healthy man who underwent an apparent recurrence of COVID-19, after three weeks of fatigue, he started feeling "completely overwhelmed" and for the next 72 hours, he "felt unwell in a way that was bordering on not coping."
He says he "felt physically exhausted" and "mentally drained." Severe illness will do that. He says it took him nearly eight weeks before he started feeling "close to my normal self again," but even then, he still struggled with "fatigue to the point of having to sleep in the day" and an inability to exercise.
COVID-19 'Long-Haulers'
He's not alone in reporting such symptoms. An estimated 10% of patients treated for COVID-19 report fatigue, breathlessness, brain fog and/or chronic pain for three weeks or longer.4 This phenomenon occurs even among patients who had mild cases of COVID-19.
U.S. Centers for Disease Control and Prevention data5 show the rate of COVID-19 patients who continue experiencing lingering health problems after recovering from acute COVID-19 may be as high as 45%. Only 65% report having returned to their previous level of health within 14 to 21 days after receiving a positive test result.
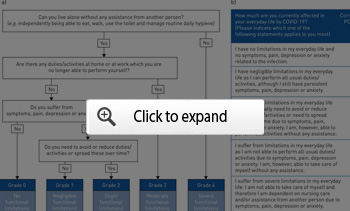
The flowchart6 below, published in the European Respiratory Journal, is a tool you can use to measure your functional status over time after recovery from COVID-19.
Treatment Guidance for Post-Acute COVID-19
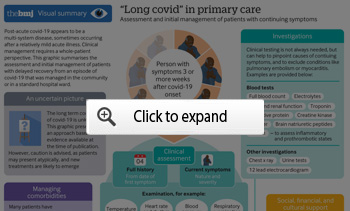
The good news is that, according to an August 11, 2020, article in The BMJ,7 which provides post-acute COVID-19 primary care guidance, many of these "long COVID" patients do spontaneously recover — albeit slowly — "with holistic support, rest, symptomatic treatment and gradual increase in activity." To support recovery, the article suggests that:8
"… patients should be managed pragmatically and symptomatically with an emphasis on holistic support while avoiding over-investigation. Fever, for example, may be treated symptomatically with paracetamol or non-steroidal anti-inflammatory drugs.
Monitoring functional status in post-acute COVID-19 patients is not yet an exact science. A post-COVID-19 functional status scale has been developed pragmatically but not formally validated9 …
Referral to a specialist rehabilitation service does not seem to be needed for most patients, who can expect a gradual, if sometimes protracted, improvement in energy levels and breathlessness, aided by careful pacing, prioritization, and modest goal setting.
In our experience, most but not all patients who were not admitted to hospital recover well with four to six weeks of light aerobic exercise (such as walking or Pilates), gradually increasing in intensity as tolerated. Those returning to employment may need support to negotiate a phased return."
The following graphic from that BMJ article10 provides a visual summary of the recommended assessment and management recommended for patients with lingering symptoms after recovering from acute COVID-19.
Chronic Fatigue in the Limelight
As reported by Time magazine,11 that many COVID-19 patients report lingering fatigue, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) has gained new attention. It seems many of these post-acute COVID-19 patients fit the diagnostic criteria for ME/CFS, which has been linked to viral infections.
For years, people with ME/CFS were disregarded as faking it. Many were told it was "all in their head." The fact that COVID-19 patients are now reporting the same problem strengthens the theory that ME/CFS really is rooted in some sort of chronic infection.
"There is … a critical mass of long-haulers getting sick and speaking out all at once, enough to draw attention from scientists, the media and the general public," Time magazine writes.12
"Enough of these patients tested positive for COVID-19 or its antibodies to make a strong case that coronavirus is turning into ME/CFS … The influx of new patients could go a long way toward figuring out why, exactly, a viral illness can last forever.
Though there are multiple theories in the ME/CFS research world, [Dr. Anthony] Komaroff [who treats ME/CFS at Brigham and Women's Hospital in Boston] believes the cause of the condition can be traced back to a part of the brain that kicks on when you're sick — the part that saps your energy and appetite so your body can focus all its energy on clearing an infection.
'This center in the brain gets flicked on, but for whatever reason it never gets switched off,' Komaroff says. New research efforts spurred by the pandemic could help determine if that's really happening, and why."
In May 2020, Maryland Rep. Jamie Raskin introduced a bill13 to provide funding to study the connection between SARS-CoV-2 and ME/CFS. The bill, HR 7057 (The UCS ME/CFS Act) has not yet cleared the U.S. House of Representatives. It has no corresponding bill in the Senate. However, studies are already underway, and "COVID-19 longhaulers" can volunteer for them on the You + ME registry.14
A significant hurdle remains though: Few doctors are familiar enough with ME/CFS to treat these patients. If the pandemic results in a massive influx of ME/CFS patients, the medical system will be ill equipped to handle it and countless patients are bound to suffer without much hope. According to Time magazine:15
"[Dr. Ron] Tompkins [a surgeon from Massachusetts General Hospital who researches ME/CFS] adds that any progress for ME/CFS patients will hinge on doctors definitively determining that coronavirus can turn into ME/CFS, rather than making post-coronavirus syndrome a separate diagnosis.
'It would be a disservice to make post-COVID something special,' he says, because ME/CFS patients wouldn't share the benefits. 'I don't think there's a nickel of difference between the two,' he adds."
The Gut Connection
While conventional medicine has no cure to offer ME/CFS patients, there's compelling evidence suggesting your gut health can play a significant role in this condition. Research published in 2017 linked both chronic fatigue and Parkinson's to gut bacteria.
People with ME/CFS have distinctly different gut microbiomes than healthy controls,16 as determined by serial sequencing of bacterial RNA, and research17,18 has found 35% to 90% of ME/CFS patients "report abdominal discomfort consistent with irritable bowel syndrome."
In related news,19 researchers have also discovered a link between COVID-19 and gut problems. A likely reason for this is because SARS-CoV-2 uses the ACE2 receptor to gain entry into the cell, and the greatest number of ACE2 receptors are found in the cells that line your gut.
According to one review,20 18.6% of COVID-19 patients had gastrointestinal symptoms such as diarrhea, nausea and vomiting. In another study,21 as many as 50.5% of COVID-19 patients admitted to the hospital had one or more digestive symptoms.
Abdominal pain is rare at just 1.9%,22 and theories of why COVID-19 would cause stomach pain include inflammation of the nerves in the gut23,24 and/or sudden loss of blood supply to abdominal organs resulting in tissue death.25
Incidentally, your gut microbiome is also known to influence your mental health, and has been linked to depression26 and anxiety,27 and a large portion of your immune system also resides in your gut.
All of these links between viral infection, gut problems, mental health issues, immune function and ME/CFS suggest restoring your gut health may be a crucial strategy if you come down with COVID-19.
How to Boost Your Gut Health
To optimize your gut microbiome, consider the following recommendations. Also keep an eye out for my interview with health scientist Rodney Dietert, which will be published shortly. In it, we discuss the connections between COVID-19 and gut health and review the importance of your gut for a well-functioning immune system.
• Avoid processed vegetable oils (polyunsaturated fats or PUFAs), as they promote inflammation, damage your endothelium (the cells lining your blood vessels) and your mitochondria, and lower your antioxidant defenses by stripping your liver of glutathione. For more details, see "The Case Against Processed Vegetable Oils."
• Avoid processed foods and conventionally raised meats and other animal products as they are routinely fed low-dose antibiotics and genetically engineered feed grown with glyphosate, which is known to kill many beneficial bacteria.
• Increase your soluble and insoluble fiber intake. Short-chain fatty acids produced by bacteria that feed on plant fiber are major epigenetic communicators. In other words, they actually communicate with your DNA, thereby providing protection against a number of different diseases. If using a fiber supplement, make sure its unprocessed, such as organic whole husk psyllium. Processed supplement fiber does not provide gut bacteria with what they need.
• Avoid chlorinated and/or fluorinated water and antibacterial soap as all will kill off healthy bacteria.
• Eat plenty of traditionally fermented foods such as lassi, natto, fermented vegetables and fermented grass fed organic milk products like kefir and yogurt, and/or take a probiotic supplement. This is particularly important after a course of antibiotics.
Additional Advice for ME/CFS and 'COVID-19 Long-Haulers'
In addition to addressing your gut health, there are many other strategies that can be helpful for ME/CFS, and yet others that appear extremely beneficial for the prevention and treatment of COVID-19 specifically. Important treatment strategies for ME/CFS include but are not limited to:
- Exercising according to your ability, with a focus on increasing the amount of exercise you can handle. Gentle exercise such as yoga can also be an excellent part of your program, and yoga benefits your mind as well as your body.
- Supplementing with nutrients important for cellular energy synthesis, such as ubiquinol, the reduced form of CoQ10, and D-ribose, a core building block of ATP.
- Eating foods rich in glutathione precursors, sulfur and selenium to encourage glutathione production. Glutathione is one of your body's most important antioxidants and a natural detoxification agent. Glutathione deficiency also appears to play a distinct role in COVID-19 and has been linked to increased severity.
- Implementing a time-restricted eating schedule so that you're eating all of your meals within a six- to eight-hour window. Also make sure your last meal is taken at least three hours before bedtime. The rationale for avoiding late night eating is directly tied to the way your body produces energy.
- Addressing your mental outlook. I recommend trying the Emotional Freedom Techniques (EFT) to help normalize your bioenergetic circuitry. Emotionally traumatic events can leave "energy blockages" for many years, which then interfere with your overall health, including immune function. There are many different techniques that can be used, but EFT is my favorite, and it's easy to learn and apply.
Lastly, recommendations that can be helpful to prevent and treat COVID-19, both in the short and long term include the following. Some of these also tie in with ME/CFS while other don't:
• Improve your insulin sensitivity by adopting a diet high in healthy fats and low in processed carbs, implementing a time-restricted eating schedule and avoiding food for at least three hours before bed.
Research shows insulin resistance is a primary and independent risk factor for severe COVID-19, which makes sense when you consider it both increases inflammation and lowers immune function. You can learn more about all of this in "The Real Pandemic Is Insulin Resistance."
Ketones — produced when you eat a cyclical ketogenic diet and/or intermittently fast — also appear to be very helpful against COVID-19, which adds further support for these lifestyle strategies.
• Supplement with:
◦ Lumbrokinase, an enzyme that helps combat blood clots (another symptom associated with more severe COVID-19) and breaks down biofilms associated with Lyme disease, an infection also linked to ME/CFS.
◦ Quercetin and zinc. Like hydroxychloroquine, quercetin helps shuttle zinc into the cell, thereby stemming viral replication. COVID-19 patients with low zinc levels have a higher risk of poor outcome and death.28
Quercetin also boosts type 1 interferon, which signals infected cells to produce proteins that stop the virus from replicating. In addition, quercetin works synergistically with vitamin C, which is another powerful COVID-19 prophylactic.
◦ Vitamin D. More than 80% of COVID-19 patients are vitamin D deficient, and the evidence overwhelmingly supports the idea that raising your vitamin D level above 40 ng/mL can go a long way toward preventing SARS-CoV-2 infection, reducing severity, lowering the risk of death and improving outcomes overall.
• Use nebulized hydrogen peroxide. Nebulizing hydrogen peroxide into your sinuses, throat and lungs is a simple, straightforward way to augment your body's natural expression of hydrogen peroxide to combat infections and can be used both prophylactically after known exposure to COVID-19 and as a treatment for mild, moderate and even severe illness.
Buy a desktop nebulizer and stock food-grade hydrogen peroxide and some saline. That way, you have everything you need and can begin treatment at home at the first signs of a respiratory infection. Keep in mind food grade hydrogen peroxide must be diluted down to a 0.1% dilution before use.
No comments:
Post a Comment