Marked Decrease in Hospital Admissions During COVID Pandemic
Published May 11, 2020 | Opinion
A curious thing is happening amid the COVID-19 pandemic: As COVID-19 cases and deaths mount, hospital admissions for other acute ailments are markedly dropping.
In an Apr. 6, 2020, New York Times article, Dr. Harlan Krumholz—professor of medicine at Yale and director of the Yale New Haven Hospital Center for Outcomes Research and Evaluation—notes:1
The hospitals are eerily quiet, except for COVID-19. I have heard this sentiment from
fellow doctors across the United States and in many other countries. We are all asking: Where are all the patients with heart attacks and stroke? They are missing from our hospitals.
Yale New Haven Hospital, where I work, has almost 300 people stricken with COVID-19, and the numbers keep rising—and yet we are not yet at capacity because of a marked decline in our usual types of patients.
In more normal times, we never have so many empty beds … What is striking is that many of the emergencies have disappeared.
Drastic Reduction in Emergency Admissions
In an informal Twitter poll, created by Angioplasty.org, an online community of cardiologists, 45.4 percent reported a 40 percent to 60 percent reduction in hospital admissions related to heart attacks, and 22.4 percent reported a reduction greater than 60 percent.2 Other emergencies, including acute appendicitis and gallbladder disease have also dropped, according to unofficial reports from medical professionals.3 What’s more, according to Krumholz:4This is not a phenomenon specific to the United States. Investigators from Spain reported a 40 percent reduction in emergency procedures for heart attacks during the last week of March compared with the period just before the pandemic hit.We still do not have an explanation for these statistics. Krumholz hypothesizes that patients may be avoiding face-to-face medical care for fear of contracting COVID-19. If this is the case, their condition may significantly worsen, and lives may be unnecessarily lost. “As we fight coronavirus, we need to combat perceptions that everyone else must stay away from the hospital. The pandemic toll will be much worse if it leads people to avoid care for life-threatening, yet treatable, conditions like heart attacks and strokes,” Krumholz says.
This isn’t the only possibility, however. As Krumholz notes, natural triggers of heart attacks and strokes may simply have been removed by the imposed social distancing, eating at home and having more time for physical activity.
He’s not convinced that this theory is the most likely explanation, though, considering respiratory infections tend to increase the risk of heart attack. The fear and stress of the situation should theoretically also have led to an increase in heart attacks, as depression, anxiety and frustration “are all associated with a doubling or more of heart attack risks.”5
Delaying Necessary Care Could Cost You
The same story is also reported in an Apr. 19, 2020, article6 in The Washington Post, which notes that:Five weeks into a nationwide coronavirus lockdown, many doctors believe the pandemic has produced a silent sub-epidemic of people who need care at hospitals but dare not come in.
They include people with inflamed appendixes, infected gall bladders and bowel obstructions, and more ominously, chest pains and stroke symptoms, according to these physicians and early research …
At [the Medical University of South Carolina, trauma medical director Dr. Evert] Eriksson’s general surgery floor, which has 20 beds, housed as few as three people for two to three weeks, he said. Now the census is back over 20.
‘What we’re seeing is late presentation,’ he said. ‘I would say 70 percent of the appendicitis on my service right now are late presentations. What happens when you present late with appendicitis is we can’t operate on you safely.’
All-Cause Mortality Is Still Uncertain
Whatever the reason for the drastic decreases in hospital admissions for ailments other than COVID-19, time will tell whether the decrease has actually resulted in increased all-cause mortality or not. As reported by The Washington Post:7Much of the reporting about missing patients is anecdotal—in medical chat rooms and on doctors’ social media accounts. Doctors say it’s unlikely there has been a decline in most of these conditions, which suggests that at least a few people may be dying at home, although there is no data yet to corroborate that.Some do claim all-cause mortality has risen during this pandemic. According to an Apr. 14 report by The New York Times:8
Three thousand more people died in New York City between Mar. 11 and Apr. 13 than would have been expected during the same time period in an ordinary year, Dr. Oxiris Barbot, the commissioner of the city Health Department, said in an interview.
While these so-called excess deaths were not explicitly linked to the virus, they might not have happened had the outbreak not occurred, in part because it overwhelmed the normal health care system.The New York Times’ claim that the deaths occurred as a result of COVID-19 “overwhelming the health care system” seems suspect, however, in light of so many doctors saying their hospitals are nowhere near capacity.
These conflicting reports show just how difficult it is to tease out the truth without proper data collection and distribution. Without accurate and complete data, it’s virtually impossible to draw any definitive conclusions.
Is Mortality Actually Going Down?
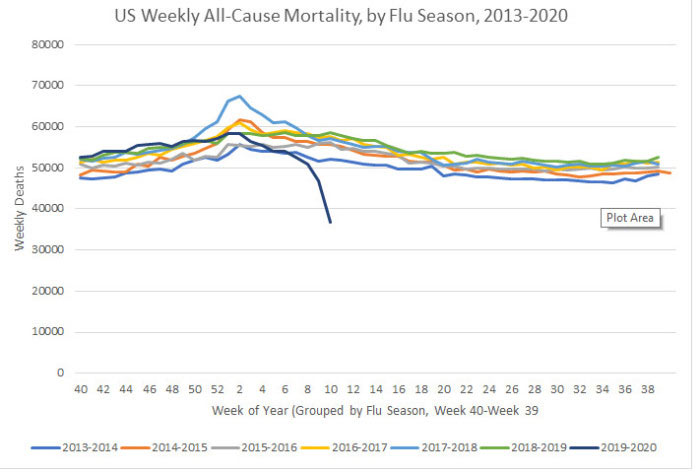
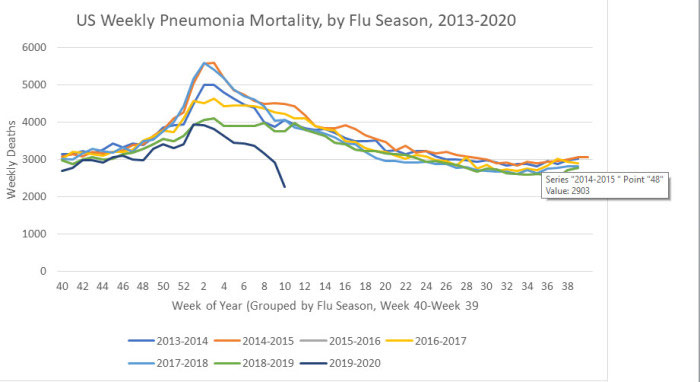
Two interesting graphs created by I. Ratel9—who freely admits he’s not a statistician or doctor but has degrees in industrial management and automotive technology and whose interest in this is fueled by the fact that he’s immunocompromised—suggest a downturn in both pneumonia deaths and all-cause mortality.Although final data won’t be released until 2021, I did find in my own research that pneumonia deaths in the current flu season (2019-20) are down compared to 2018-19,10 so I’m including Ratel’s calculations here for anyone interested in diving deeper into his data gathering. Ratel explains the graphs:11
I’ve been watching CDC’s flu surveillance since last fall when there were rumors floating about of a nasty new flu bug in China … According to the South China Post, the first COVID-19 case in Hubei province China was found November 17. Even that article states that patient zero may have been earlier than that …
I contend that it is reasonable to believe that the SARS-CoV-2 virus began circulating around the global population back in November and December, spreading not only across China, but to much of the world.
When considering that possibility, patterns in CDC’s regular ILI (Influenza Like Illness) surveillance data become interesting. I’ve taken their data, and applied my meager Excel skills to chart out some things …
Prior to January we weren’t looking for this virus. We’ve only had useful testing capability for a few weeks now. Given the information we have on disease progression, I assumed that there would be an upward trend in Pneumonia mortality as without looking for and testing for SARS-COV-2, victims should have been classified as deaths due to pneumonia. So, I charted it, with the last 6 years of data published by CDC.
CDC calls week 40 of a year the beginning of the flu season, so all my charts are set to begin in week 40 of one year and end in week 39 of the next, showing years as flu seasons.
Avoiding Hospitals Might Lower Death Toll
That said, previous research has shown that when conventional medical intervention is reduced, mortality often goes down. For example, back in 2000, all-cause mortality in Israel dropped during a time when Israeli doctors at public hospitals went on strike.12One of the reasons for this is because medical care itself tends to be a risky business. Research13 published in 2014 found nearly 1 in 5 elderly Medicare patients are injured by their medical care. The most common medical injuries included receiving the wrong medication, having an allergic reaction to medication given, and receiving treatment that led to more complications. As a result of these injuries, they also had a death rate nearly double those who were not injured by their care.
Other research14 published in 2013 concluded 210,000 Americans are killed by preventable hospital errors each year, and when deaths related to diagnostic errors, errors of omission, and failure to follow guidelines were included, the number skyrocketed to an estimated 440,000 preventable hospital deaths each year.
One in 25 patients in the U.S. also contracts some form of infection while hospitalized, and an estimated 205 Americans die from hospital-acquired infections every day. The unfortunate truth is that once you’re hospitalized, you’re immediately at risk for medical errors that might cost you your life. That’s not to say you should never go to the hospital, though.
If you suspect you’re having a heart attack, stroke or appendicitis, for example, you should seek immediate care. Many other ailments that people seek treatment for, however, may simply place them at increased risk for complications.
The difficulty is determining what you might be able to address at home and what’s an actual emergency. If you have access to a holistic physician you trust, calling them for a consultation would be a good idea.
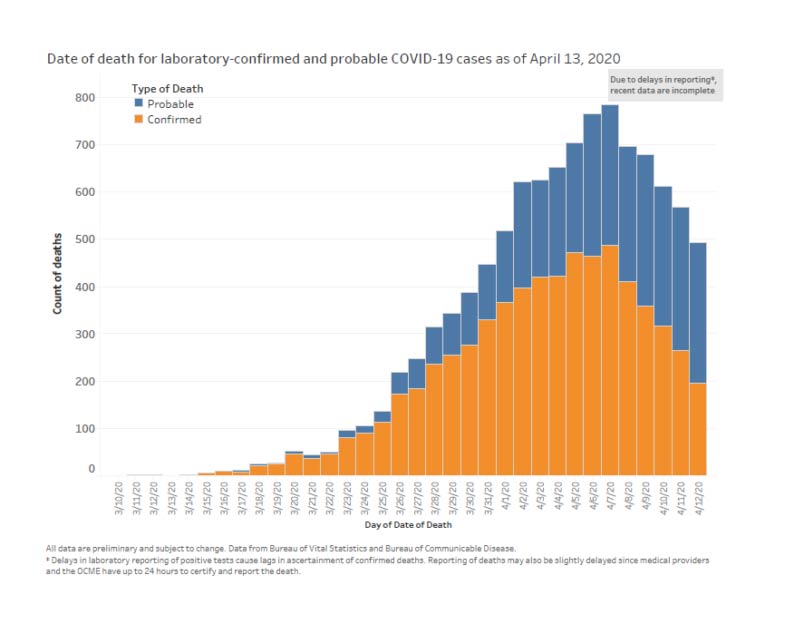
COVID-19 Deaths Jump Due to Reclassification
While other ailments appear to have declined (at least based on hospital admission rates, which may present a false picture of the situation), COVID-19 deaths in the U.S. have undergone a sudden jump mid-April.While some use this as a sign that the infection is spreading and perhaps more lethal than suspected, the real reason for this sudden jump is simply the reclassification of COVID-19 deaths to include “probable” cases.
While the U.S. Centers for Disease Control and Prevention15 separates confirmed COVID-19 deaths from all-cause mortality, pneumonia deaths, influenza deaths and deaths with both pneumonia and COVID-19, it has issued guidance to states on how to document COVID-19 deaths on death certificates, indicating that COVID-19 should be indicated if “the disease caused or is assumed to have caused or contributed to death.”16
By not requiring COVID-19 deaths to be laboratory confirmed, the death rate can easily become skewed. New York City has officially transitioned its record keeping to include suspected COVID-19 cases,17 18 and as you’d expect, when suspected or “probable” deaths are counted without any proof that SARS-CoV-2 infection was involved at all, the numbers dramatically increase. Ultimately, there is no way to tell what the real impact of the pandemic actually is when using this system.
Looking at the data19 collected for NYC between Mar. 11, 2020, and Apr. 13, 2020, 23.5% of deaths involving residents between the ages of 45 and 64 are in the “probable” category, as are 23.6% of those among 65- to 74-year-olds and 49.9 percent of those over the age of 75.
As noted by The New York Times20 on Apr. 14, 2020, New York City’s addition of thousands of “probable” cases increased the alleged death rate from COVID-19 by 17 percent overnight.
Signs of Suicide Epidemic Emerge
Whether all-cause mortality is in fact going up or down, as predicted we are now starting to see a rise in suicides. Suicide statistics reliably follow economic trends, with financial downturns triggering higher rates of depression and despair. According to an updated Mar. 27, 2020, report by The Sacramento Bee:21FirstLink, a company that answers both 211 helplines and the National Suicide Prevention Lifeline for North Dakota and parts of Minnesota said this week that call volume in some of its call centers is up 300%.According to a spokeswoman for the national Crisis Text Line, text conversations were double that of the normal volume during the week of Mar. 15.22 Google also reports that searches for “panic attack symptoms” have doubled compared to last year.23
The CDC, meanwhile, appears to take things in stride, noting that “Fear and anxiety about a disease can be overwhelming and cause strong emotions in adults and children,” but that “Coping with stress will make you, the people you care about, and your community stronger.”24
While true as a general statement, the current pandemic has delivered a perfect storm of challenges that is sure to bring many to a breaking point. We’re not just talking about fearing a disease. We’re also talking about the very real challenges of keeping a roof over our heads and feeding ourselves and our families when the entire country has been shut down and millions of workers have been laid off.
According to reports by The Federalist25 and Red State,26 suicides exceeded COVID-19 deaths in Tennessee the week of Mar. 20. The Regional Forensic Center in Tennessee was investigating nine suicides as of Mar. 27, eight of which took place in Knox County—one of the few areas in Tennessee where businesses were ordered to close.
The suicides, which occurred within a 48-hour period, account for 10% of the 2019 suicide rate for the region.27 Meanwhile, only six patients died from COVID-19 in the entire state that week. In a statement, Knoxville, Tennessee Mayor Glenn Jacobs said:28
That number is completely shocking and makes me wonder if what we are doing now is really the best approach. We have to determine how we can respond to COVID-19 in a way that keeps our economy intact, keeps people employed and empowers them with a feeling of hope and optimism—not desperation and despair.Similar warning signs are starting to be noted in other states as well, including Oregon. In a Mar. 24 local news report,29 Portland police chief Jami Resch said suicide threats or attempts are 41 percent higher now than this time last year, and there’s been a 23 percent increase since the 10 days before a state of emergency was declared in Portland.
Unfortunately, this is likely the beginning of what is most certainly only going to worsen with time, as many financial experts are predicting a depression worse than the Great Depression of the 1930s.30
This article was reprinted with the author’s permission. It was originally published on Dr. Mercola’s website at www.mercola.com.
References:
No comments:
Post a Comment