What We Aren't Told About OsteoporosisHow conventional osteoporosis care often makes things worse and the forgotten ways to regain bone health.Story at a Glance •A
gradual weakening of the bones which predisposes one to fractures is
one of the most common and significant consequences of aging. Presently,
to address it, we wisely try to head off bone loss in our younger years
and routinely scan the density of aging bones so that a large volume of
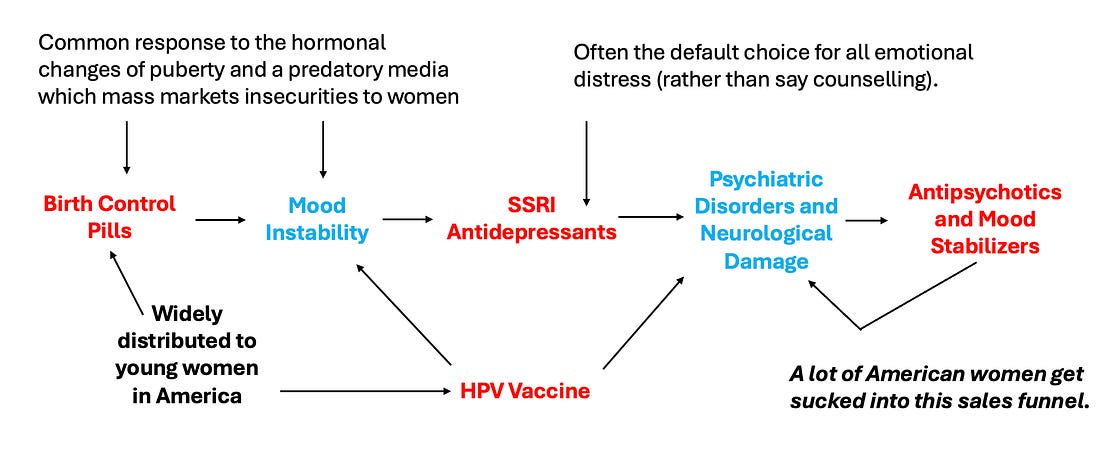
patients can be sold drugs to increase bone density. •Because of this, there is relatively little knowledge of the actual causes of osteoporosis or the most effective ways to restore the strength of the bones. The causes and treatments of osteoporosis will be the focus of this article. Note: one of my favorite things about publishing on Substack is that I can continually revise articles as I learn new information (e.g., much has been added to the existing DMSO articles). As such, I periodically republish revised versions of the articles readers here found to be the most helpful and it is my aim to eventually unmask each of the commonly prescribed drugs that cause a lot of problems. The years I have spent studying the medical industry have made me appreciate how often economic principles can allow one to understand its complex and contradictory behavior. For example, I believe many of the inconsistencies in medical ethics (e.g., “mothers have an absolute right to abort their children” and “mothers cannot refuse to vaccinate their children because it endangers their child’s life”) can be explained by simply acknowledging that whatever makes money is deemed “ethical.” Sales FunnelsIn my eyes, one of the most important business principles for understanding medicine are sales funnels,
a method of selling products where you initially cast a wide net, and
then successively cast smaller nets for increasingly expensive products
after catching your initial customers. I typically see two types of (often overlapping) sales funnels in medicine. Note: a good case can be made that many of the chronic illnesses our children suffer from now (which are very lucrative to “treat”) are a direct consequence of the ever increasing number of vaccines in the marketplace. The
second funnel works by recasting “preventative medicine” and “promoting
health” as the task of screening for each person for conditions they
are at risk for. The results from these universal screenings are then
used to justify selling them medical services (e.g., drug
prescriptions). Once that screening becomes normalized, the industry
will then pivot to expanding the funnel and having far more services be
sold. For example: Note: the folly of this approach is highlighted by a trial which found removing on average 2.8 non-essential drugs from the elderly at one facility caused their 1 year death rate to go from 45%-21% and their hospitalizations that year to go from 30%-11.8%. As far as I know, there is no intervention on the market which offers a benefit comparable to this. Radiographic ScreeningsOne of the common ways mass screenings are done is through giving lots of patients X-rays and then funneling those with abnormal imaging into being treated. For
example, women over the age of 50 are advised to get a mammogram every
two years so that their deadly breast cancers can be identified and the
women can be saved through early treatment for the cancers. However,
whenever these screening programs are studied, they are found to not
provide a net benefit because: Peter Gøtzsche
in turn conducted an exhaustive review of the evidence on routine
mammogram screening which should have ended the practice (it can be read
here).
However, his data (which was widely publicized) had no effect on these
screening programs. Many (myself included) believe that was because
radiologists make so much money from mammograms they have an inherent
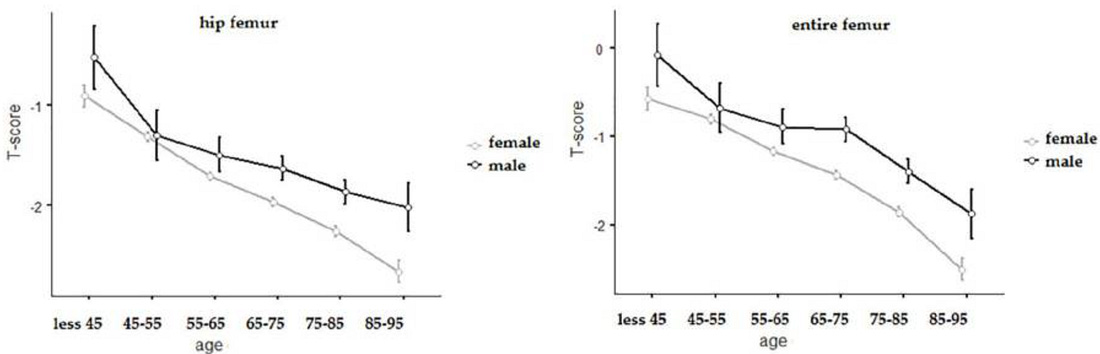
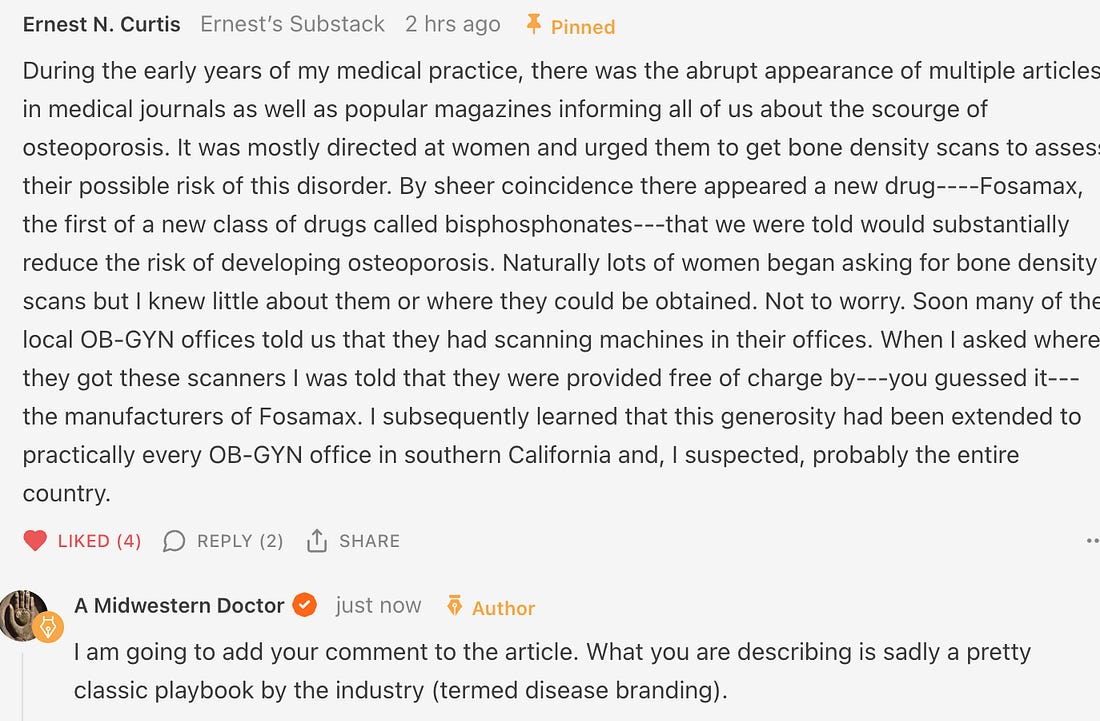
need to justify the necessity of this routine screening. DEXA ScamsAnother universal screening practice for women are dual energy X-ray absorptiometry (DEXA) scans, which calculate the density of bones and hence are believed to be a proxy for bone strength. It is then compared to the average bone density of a 30 year old, and a statistical method is applied to determine how far away their density is from that value which then produces their T-score. Every medical student in turn is taught that a T-score of 0 to -1 is normal, -1 to -2.5 is on the way to being bad (osteopenia) and a T-score that is -2.5 or worse means your bones are weak enough that you have osteoporosis and must urgently begin treatment for it. If you take a step back, a few questions should come to mind. First, since bones naturally become less dense with age, most people will have bones that are less dense than those of a 30 year old. In turn, the current of management of osteoporosis accepts that bone loss is inevitable and reasonably tries to prevent that loss early on since it is so much harder to regain it later in life. Hence, many people due to the normal process of aging will have osteopenia or osteoporosis. Consider for example what this study concluded was the average T-score by age of Italians. Note: if, for instance, the average T-score for a group is -2.5, this will mean a lot of people within that group (half of them) will have a score below -2.5 and conversely, at lower “averages” even more will have osteoporosis. Additionally, T-scores are calculated utilizing the standard deviation of the bone densities in 30 year olds, a value which can be up to 50% smaller than that of older adults (making it much easier to pass the -2.5 threshold). Second, how accurate are the scans? As it turns out, there is actually a great deal of variance in DEXA scan results depending on which machine is used, how the operator performs the test and what bones are measured, with studies often finding
a 5-6% difference in bone density depending on where the test was done.
More importantly, since the T-score is based off standard deviations, a
5-6% difference in bone density can, in turn, change the T-score by
0.2-0.4 (which equates to a decade of bone loss) and hence tip many over
to an osteoporosis diagnosis. Third, is there any point to repeatedly doing them? As it turns out, a study of 4124 older women found that once an initial DEXA result was obtained, there was no additional information of use gained from repeating the study over the next 8 years. Nonetheless, many guidelines often recommend getting a scan every 1-2 years, and likewise, Medicare pays for one every 2 years. As these scans typically cost between $150 to $300, that quickly adds up. Fourth, do the scans accurately reflect bone strength and the risk of fractures? While they are generally predictive of the risk, they are not as accurate as is commonly believed. For example, this study found the osteoporosis status of a patient (determined by their T-score) frequently did not match what was directly observed within bones under a microscope. Similarly, this study found that when bones were deliberately weakened, Dexa scans underestimated how much strength had been lost. Note: a cheaper method of diagnosing bone strength (which does not expose patients to ionizing radiation) is beginning to be used in Europe. It works by sending ultrasound waves into bone and then analyzing the spectrum created by those waves to assess the health of the bones. As the attached presentation shows, it accurately predicts bone density, and additionally, predicts bone strength. In short, this may be a dramatically superior approach to Dexa scans, but it is unlikely we will see it enter regular use in the United States for at least a decade due to how heavily invested many already are in performing Dexa scans. Note: the story above in the comment is discussed in more detail in this NPR article. BisphosphonatesOnce a patient is diagnosed with osteoporosis (and in some cases after an osteopenia diagnosis), the first line treatment is to start a bisphosphonate and continue it for up to 3-5 years depending on if the drug is administered intravenously or orally. A variety of factors influence the development of bone. Two of the most important ones are the cells that build bone up (osteoblasts) and the cells that break bone down (osteoclasts). Bisphosphonates in turn concentrate in the bone and work by disabling or killing osteoclasts. This thus leads to bone density increasing because the balance of bone production shifts towards building them up rather than breaking them down. Unfortunately, there are two problems with this approach. 1. Bisphosphonates are notorious for having a large number of side effects. Commonly recognized ones include:
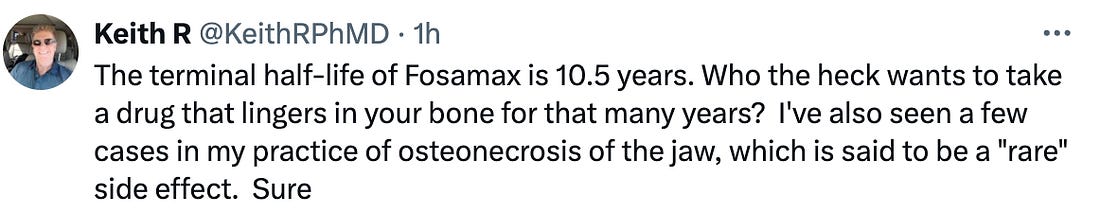
To illustrate, a January 2008 FDA alert, warned physicians that all bisphosphonates may cause:
Note: we also find a variety of other significant issues occur. For example, we’ve seen many patients on bisphosphonates develop bone spurs in the jaw (which can be quite challenging for them to deal with). Similarly, a study of individuals who have had fractures after 3-8 years of bisphosphonate usage discovered that they had almost no new bone formation occurring. 2. The way bisphosphonates work is very different to how the body was designed to build healthy bone, and in effect, much of the bone they leave you with is “old bone.” Note: a variety of other newer drugs exist to treat osteoporosis. These drugs are often more effective at producing stronger bones, and often don’t have the same significant side effects seen with the bisphosphonates, so quite a few of my colleagues use them. Unfortunately, those drugs tend to be much more expensive and each one still has its own set of side effects. Physiologic MomentumOne of the most remarkable aspects of the human body is its ability to gradually adapt to whatever circumstances it finds itself in. Conversely, one of the primary challenges one faces when dealing with a chronic illness is that typically by the time the symptoms of the disease emerge, the maladaptive physiologic process that gave rise to those symptoms is firmly established within the body and hence quite difficult (and time consuming) to shift. For example, Alzheimer’s disease typically is a result of the processes which create neurons slowing down and being outpaced by the processes that destroy them, hence leading to an increasing neuronal loss and an increasing loss of neurological function. In turn, the only method which has ever been proven to treat Alzheimer’s is to simply reverse that equation and have neuronal production outpace neuronal destruction. Unfortunately, since a drug can’t be made to do that (rather it requires changing one’s lifestyle) the industry has instead relentlessly focused on drugs which eliminate the plaque the brain forms to protect its neurons from injury. Thus all we have to show after decades of spending billions each year to find a cure for this disease are expensive plaque targeting that have a wide range of side effects and are useless for actually treating Alzheimer’s disease. One of the most important adaptive processes in the body is how it accommodates to the stresses and loads placed upon it. For example, the reason why weight training “works” is because muscles being stressed through overexertion gives a signal to the body that it needs to build more muscle. However,
while the adaptive process with muscles is frequently recognized, many
others are not. For instance, the body continually remodels the soft
tissue which connects the body together, and as a result, when someone
experiences a pharmaceutical injury which damages the body’s ability to
rebuild those tissues, they are likely to subsequently experience a
critical structural failure. Bone RemodelingAn adaptive process also continually reshapes the bones so that their architecture is arranged to optimally bear the loads placed upon them. In most cases, we never think about this process because it just works as intended. However, in certain cases, we do recognize where it has gone awry. For example, since the bones depend upon the weight of gravity for the signal to be built up (via the electrical currents that are created when bone is compressed), that signal is lost in low gravity environments. Because of this, a longstanding problem in space travel was the rapid bone loss astronauts experienced (e.g., in 6 months they lost 6-10% of their bone density, which put them at a high risk for fractures once they returned to normal gravity and typically took 3 or more years to recover from). Because of this, while we typically only focus on the cells which build bone, the reality is that the osteoclasts are also immensely important, as their destruction of bone is what allows bone to assume the shape which best allows it to effectively bare the weight of gravity. In turn, when they are blocked by a bisphosonate, bone density increases, but the bones that form are much more brittle and inflexible. Our dislike of those drugs in turn comes about from how frequently we encounter the pathologic changes they create in our patient’s bones (e.g., we find that while compressive strength may be increased, bone mobility is not, and that is often far more consequential for the patients). This in turn highlights a common problem in medicine. Frequently doctors are trained to focus on treating numbers (e.g., reducing a “high” cholesterol) under the belief that correcting those numbers creates health. Much of this comes from the fact it’s much easier to conduct a study that assesses benefit through the change of a value which is assumed to be good (e.g., a vaccine creating the target antibodies) than it is to evaluate if an actual improvement occurs for patients (e.g., a decrease in the total number of people who died—which in Pfizer’s studies did not occur despite the fact “lifesaving” antibodies were consistently being produced). In short I would argue that while bisphonates may be effective at improving a DEXA score, they aren’t necessarily good at improving health. What Causes Osteoporosis?Since bone metabolism is linked to many other processes in the body, a variety of things can affect it. In turn, I find that colleagues who focus on treating a specific aspect of the body are often able to provide proof their area of focus is the primary determinant of bone health. This hence makes it quite challenging to establish which area is in fact matters most. That said, there are a few factors of particular importance. 1. Mobility—since
bone growth depends upon the signals generated from loading weight on
the body, a good case can be made that our increasingly sedentary
lifestyles are responsible for the continual increase in osteoporosis occurring in America (e.g., one study
found sedentary postmenopausal women lost 2.26% of their bone mass in a
year, while those who did a weight training program instead had a 1.17%
increase). Additionally, sunlight exposure has been shown to increase bone density (along with providing many other critical health benefits), which further illustrates how problematic being sedentary inside can be. This in turn argues that hormones play a vital role in bone health, and in turn, the hormonal medicine field frequently prescribes estrogen to older women to compensate for the loss of estrogen which accompanies menopause, partly under the belief that hormonal supplementation can hence prevent menopause. However, while supplemental estrogen appears to help prevent bone loss, we don’t focus on this approach because: •In our experience, the most important thing is not the bone’s density, but rather its elasticity and mobility. When healthy bones are subject to a loading stress, they bend to accommodate that stress and then spring back into their original shape, whereas if a bone is brittle, once it begins to bend, it will break. The primary hormone which imparts elasticity to the bones (and induces osteoblast activity) is progesterone, and like estrogen, it declines with age—particularly after menopause. In turn, we find that appropriately supplementing progesterone (which unlike estrogen is almost never dangerous), is highly effective at preventing fractures within the body. Note: osteoporosis, while rarer, also occurs in men. We find that for men, increasing testosterone levels can also help with bone loss, however the magnitude of benefit is not as much as is seen with other hormonal interventions. 3. Inflammation—many of us have observed that patients with chronic inflammatory diseases tend to be at a greater risk of osteoporosis. In turn, the mechanism to support these observations exists as the cytokines classically associated with those inflammatory disease states (e.g., TNF-α and IL-6) have been shown to activate key receptors (e.g., RANKL) which cause osteoclasts to dismantle bone until the underlying disease which is generating those cytokines is addressed. 4. Minerals—since
bones are composed of minerals, this suggests bone strength is
dependent upon the dietary intake of minerals. Our own experience has
been that supplementing with the correct minerals is often what restores
bone health, so I am inclined to believe this is indeed a critical
point. •A
stomach acid deficiency (since stomach acid is often necessary to
absorb dietary minerals). Two of the most common causes of this are acid
blocking medications (which have been repeatedly shown to cause osteoporosis) and the tendency for stomach acid to decline with age (which may in turn explain why osteoporosis increases with age). •The tendency for the widely used herbicide Roundup to behave as a chelating agent which binds essential minerals in the soil (particularly the +2 cations like magnesium) and hence prevents them from entering our bodies. 5. Water Fluoridation—Fluoride
was originally added to the water supply because it was a toxic waste
product numerous industries needed a liability free way to dispose of.
Since fluoride was known to increase bone density, this was used to
argue that it could protect our teeth, and hence that it could instead
be viewed as a vital nutrient. These attempts were initially
unsuccessful (as fluoride has a wide range of toxicities), but
eventually, since fluoride was needed to produce the original atomic bombs, for national security reasons, the government relented and added fluoride to the water supply. 7. Environmental Toxins—as the following links show, variety of widely pervasive environmental toxins (e.g., organophosphates, Bisphenol A, aluminum, cadmium and nicotine, lead, mercury, triclosans, along with many other persistent organic pollutants) can inhibit bone formation and are linked to osteoporosis. At the same time however, I’m not completely sure these points paint the full picture because the most ancient medical texts in the world also discussed osteoporosis (at a time when, for instance, Roundup and Acid Blockers did not exist) In addition to these mechanisms, there are a few others I suspect cause osteoporosis but I have less evidence to support those claims. In the final part of this article, I will list those mechanisms and our preferred protocols for treating osteoporosis (some of which, such as the minerals are quite simple, others like hormonal management are a bit complicated, along with some that are a more out of the box or that can be done in your younger years to head off a critical loss of bone mass in the future)... Continue reading this post for free in the Substack app |

No comments:
Post a Comment