June 04, 2020
LOCKDOWN LUNACY: The Thinking Person’s Guide
By J.B. Handley, CHD Contributing WriterFor anyone willing to look, there are so many facts that tell the true story, and it goes something like this:
Knowing what we know today about COVID-19’s Infection Fatality Rate, asymmetric impact by age and medical condition, non-transmissibility by asymptomatic people and in outdoor settings, near-zero fatality rate for children, and the basic understanding of viruses through Farr’s law, locking down society was a bone-headed policy decision so devastating to society that historians may judge it
as the all-time worst decision ever made. Worse, as these clear facts have become available, many policy-makers haven’t shifted their positions, despite the fact that every hour under any stage of lockdown has a domino-effect of devastation to society. Meanwhile, the media—with a few notable exceptions—is oddly silent on all the good news. Luckily, an unexpected group of heroes across the political landscape—many of them doctors and scientists—have emerged to tell the truth, despite facing extreme criticism and censorship from an angry mob desperate to continue fighting an imaginary war.
My goal is to engage in known facts. You, the reader, can decide if all of these facts, when you put them together, equate to the story above.
Fact #1: The Infection Fatality Rate for COVID-19 is somewhere between 0.07-0.20%, in line with seasonal flu
The Infection Fatality Rate math of ANY new virus ALWAYS declines over time as more data becomes available, as any virologist could tell you. In the early days of COVID-19 where we only had data from China, there was a fear that the IFR could be as high as 3.4%, which would indeed be cataclysmic. On April 17th, the first study was published from Stanford researchers that should have ended all lockdowns immediately, as the scientists reported that their research “implies that the infection is much more widespread than indicated by the number of confirmed cases” and pegged the IFR between 0.12-0.2%. The researchers also speculated that the final IFR, as more data emerged, would likely “be lower.” For context, seasonal flu has an IFR of 0.1%. Smallpox? 30%.As the first study to peg the IFR, the Stanford study came under withering criticism, prompting the lead researcher, Dr. John Ioannidis to note,
“There’s some sort of mob mentality here operating that they just insist that this has to be the end of the world, and it has to be that the sky is falling. It’s attacking studies with data based on speculation and science fiction. But dismissing real data in favor of mathematical speculation is mind-boggling.”
Like all good science, the Stanford data on IFR has now been replicated so many times that our own Centers for Disease Control came out this week to announce that their ‘best estimate’ showed an IFR below 0.3%. In this article on the CDC’s new data, they also highlighted how the cascading declines in IFR has removed all the fears of doomsday:
That “best estimate” scenario also assumes that 35 percent of infections are asymptomatic, meaning the total number of infections is more than 50 percent larger than the number of symptomatic cases. It therefore implies that the IFR is between 0.2 percent and 0.3 percent. By contrast, the projections that the CDC made in March, which predicted that as many as 1.7 million Americans could die from COVID-19 without intervention, assumed an IFR of 0.8 percent. Around the same time, researchers at Imperial College produced a worst-case scenario in which 2.2 million Americans died, based on an IFR of 0.9 percent.If you’re still unconvinced that the IFR of COVID-19 is roughly in line with a bad flu season, the most comprehensive analysis I have seen comes from Oxford University, who recently stated:
“Taking account of historical experience, trends in the data, increased number of infections in the population at largest, and potential impact of misclassification of deaths gives a presumed estimate for the COVID-19 IFR somewhere between 0.1% and 0.41%.”Finally, just last week, Stanford’s Dr. Ioannidis published a meta-analysis (because so many IFR studies have been done around the world in April and early May) where he analyzed TWELVE separate IFR studies and his conclusion is so good, I’ll just leave you with it:
The infection fatality rate (IFR), the probability of dying for a person who is infected, is one of the most critical and most contested features of the coronavirus disease 2019 (COVID-19) pandemic. The expected total mortality burden of COVID-19 is directly related to the IFR. Moreover, justification for various non-pharmacological public health interventions depends crucially on the IFR. Some aggressive interventions that potentially induce also more pronounced collateral harms1 may be considered appropriate, if IFR is high. Conversely, the same measures may fall short of acceptable risk-benefit thresholds, if the IFR is low…Interestingly, despite their differences in design, execution, and analysis, most studies provide IFR point estimates that are within a relatively narrow range. Seven of the 12 inferred IFRs are in the range 0.07 to 0.20 (corrected IFR of 0.06 to 0.16) which are similar to IFR values of seasonal influenza. Three values are modestly higher (corrected IFR of 0.25-0.40 in Gangelt, Geneva, and Wuhan) and two are modestly lower than this range (corrected IFR of 0.02-0.03 in Kobe and Oise).Opinion #1: Dr. Scott Atlas
The recent Stanford University antibody study now estimates that the fatality rate if infected is likely 0.1 to 0.2 percent, a risk far lower than previous World Health Organization estimates that were 20 to 30 times higher and that motivated isolation policies…Let’s stop underemphasizing empirical evidence while instead doubling down on hypothetical models. Facts matter.Facts do matter, but no one listened. Dr. Atlas’ article also helps frame Fact #2.
Fact #2: The risk of dying from COVID-19 is much higher than the average IFR for older people and those with co-morbidities, and much lower than the average IFR for younger healthy people, and nearing zero for children
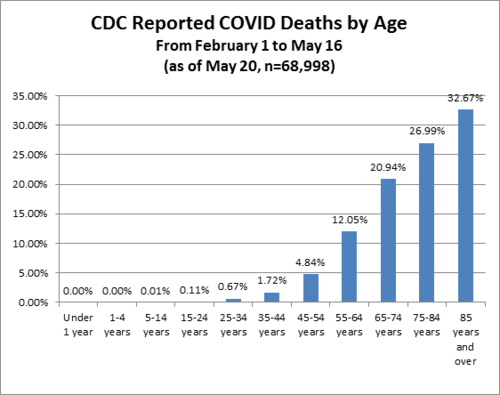
Italy reported three days ago that 96% of Italians who died from COVID-19 had “other illnesses” and were, on average, 80 years old. From Bloomberg:
“The latest numbers show that new cases and fatalities have a common profile: mostly elderly people with previous illnesses,” ISS chief Silvio Brusaferro said at a news conference Friday.The best age stratification data I have seen comes from Worldometers.info. Here’s their chart estimating death rate by age group. Please note that death rate is MUCH higher than IFR because death rate uses confirmed COVID-19 cases as the denominator, but it shows you how different the fatality rates are by age:
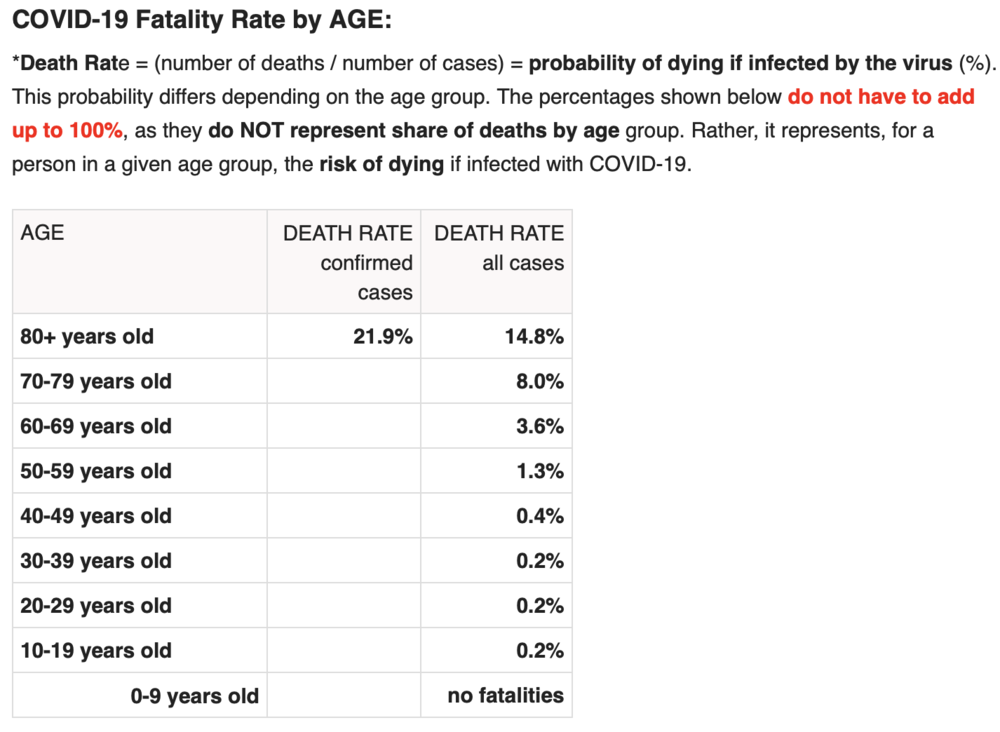
While this data is “crude”, it’s safe to extrapolate that an 80+ year-old person has a serious risk of dying from COVID-19 while a child faces almost no risk. This fact should drive policy, as Dr. Atlas explains:
Of all fatal cases in New York state, two-thirds were in patients over 70 years of age; more than 95 percent were over 50 years of age; and about 90 percent of all fatal cases had an underlying illness. Of 6,570 confirmed COVID-19 deaths fully investigated for underlying conditions to date, 6,520, or 99.2 percent, had an underlying illness. If you do not already have an underlying chronic condition, your chances of dying are small, regardless of age. And young adults and children in normal health have almost no risk of any serious illness from COVID-19.Consider this excellent article from the British Medical Journal, titled “Shielding from covid-19 should be stratified by risk” written by Cambridge University professors:
Protecting those at most risk of dying from covid-19 while relaxing the strictures on others provides a way forward in the SARS-CoV-2 epidemic, given the virus is unlikely to disappear in the foreseeable future. Such targeted approaches would, however, require a shift away from the notion that we are all seriously threatened by the disease, which has led to levels of personal fear being strikingly mismatched to objective risk of death. Instead, the aim should be to communicate realistic levels of risk as they apply to different groups, not to reassure or frighten but to allow informed personal decisions in a setting of necessary uncertainty.As one simple example: closing schools makes almost no sense given what we know about COVID-19, while protecting teachers over the age of 60—to pick a somewhat defensible age boundary—may well make sense. This is why so many countries who seem to respect data more than we do here in the U.S. have already re-opened their schools. In fact, Denmark’s schools have been open since mid-April!! And, for those keeping score, Reuters just reported yesterday that, “Reopening schools in Denmark did not worsen outbreak, data shows.” Here’s a quote:
“You cannot see any negative effects from the reopening of schools,” Peter Andersen, doctor of infectious disease epidemiology and prevention at the Danish Serum Institute said on Thursday told Reuters. In Finland, a top official announced similar findings on Wednesday, saying nothing so far suggested the coronavirus had spread faster since schools reopened in mid-May.Another great article on schools, titled, “It is fear – not science – that is stopping our children being educated” in The Telegraph newspaper last week, here’s a quote:
There is little about coronavirus we can be absolutely sure of – this is a brand new disease and our knowledge grows by the day – but most of the available evidence so far strongly suggests that children are neither suffering from coronavirus nor spreading it. Studies in South Korea, Iceland, Italy, Japan, France, China, the Netherlands and Australia all concur that youngsters are “not implicated significantly in transmitting Covid”, not even to parents and siblings.Brand new science (May 28) released from Northern Ireland clearly shows that schoolchildren do NOT serve as vectors for COVID-19. Titled, No evidence of secondary transmission of COVID-19 from children attending school in Ireland, 2020, the study could not be more clear:
Adult paranoia, stoked by over-the-top government messaging, union intransigence and media conniptions, is now being inflicted on the youngest members of our society to whom the virus poses a threat so tiny scientists call it “statistically irrelevant”. Instead of nursery rhymes, mixed infants may soon be invited to sing something called the “two-metre-song” as they stick their arms out to keep their friends at bay.
These findings suggest that schools are not a high risk setting for transmission of COVID-19 between pupils or between staff and pupils. Given the burden of closure outlined by Bayhem [4] and Van Lanker [5], reopening of schools should be considered as an early rather than a late measure in the lifting of restriction.Finally, Dr. Scott Atlas took on the topic of schools in this recent interview:
“There’s no science whatsoever to keep K-through-12 schools closed, nor to have masks or social distancing on children, nor to keep summer programs closed. What we know now is that the risk of death and the risk of even a serious illness is nearly zero in people under 18.Quick update: after I wrote this, the Wall Street Journal published this article titled Is It Safe to Reopen Schools? These Countries Say Yes. To me, this reads as a bit of a litmus test for countries that have independent and data-driven public health officials, and I give the U.S. an ‘F” for our current approach:
But Denmark, Austria, Norway, Finland, Singapore, Australia, New Zealand and most other countries that have reopened classrooms haven’t had outbreaks in schools or day-care centers…In Denmark, the opening of schools had no impact on the progress of the epidemic, said Tyra Grove Krause, a senior official with the State Serum Institute, the country’s disease control agency…Since Austria reopened on May 18, no increase in infections has been observed in schools and kindergartens, a spokesman for the government said…In Norway, the government won’t close schools again even if the number of cases starts rising in the country because there have been no negative consequences from reopening schools on April 20, said Education Minister Guri Melby.How many more countries need to re-open before the U.S. follows? Seriously, it’s a little embarrassing to be American…IMO we look like total chumps.
Update #2: Dr. Scott Atlas doubled-down on June 1st with this great Op-Ed, once again in The Hill, titled Science says: ‘Open the schools’. As usual, he’s amazingly eloquent, here’s an excerpt but well worth the time to read every word, he simply slays it:
All of this borders on the absurd, when we now know that social distancing and face coverings for children are completely unnecessary.(Special note: there’s a new boogeyman, Kawasaki disease, that some are trying to link to COVID-19. Here’s a great article about that, or see the website of the UK’s Kawasaki Disease Foundation where they discuss the “mishandling of information” about Kawasaki disease. Dr. Atlas’ most recent post discusses this, too: “What about the new threat similar to Kawasaki disease, recently sensationalized as a COVID-19 association? In fact, the association is extremely low, and the incidence of the disorder is itself rare, affecting only 3,000 to 5,000 children in the United States each year. Importantly, the syndrome is typically treatable and never has been regarded previously as a risk so serious that schools must be shuttered.”)
Never have schools subjected children to such an unhealthy, uncomfortable and anti-educational environment, so science cannot precisely define the total harm it will cause. But science does tell us that risks from COVID-19 are too minimal to sacrifice the educational, social, emotional and physical well-being – to say nothing of the very health – of our young people.
Fact #3: People infected with COVID-19 who are asymptomatic (which is most people) do NOT spread COVID-19

It’s not that easy to find people who are infected with COVID-19 but asymptomatic, because they don’t seek medical attention. Here in Oregon where I live, you can’t even get a COVID-19 test unless you have symptoms. So, the stars aligned to put this woman in a hospital with researchers studying COVID-19, and she became the subject of an extensive contact study published on May 13 in Respiratory Medicine, titled, “A study on infectivity of asymptomatic SARS-CoV-2 carriers.”
The researchers wanted to find out whether this woman, with a COVID-19 infection but no symptoms, had infected anyone else, so they chose to look at every single contact they could identify within the previous 5 days prior to her positive test. So, how many people did they have to screen? 455. Not a small number, as the researchers explain:
455 contacts who were exposed to the asymptomatic COVID-19 virus carrier became the subjects of our research. They were divided into three groups: 35 patients, 196 family members and 224 hospital staffs. We extracted their epidemiological information, clinical records, auxiliary examination results and therapeutic schedules.As you can see, being hospitalized led to the majority of the contacts this woman had, both with other patients and with many members of the hospital staff. Notably, all of these contacts took place indoors and one might argue many of the contacts—at least with hospital staff—would have involved relatively intimate contact. Amongst the patients, the average age was 62, arguably making them higher risk, and many of those patients were immunocompromised for a variety of reasons, including chemotherapy and cardiovascular disease. So how many of the 455 people were infected by the asymptomatic 22-year old woman?
“In summary, all the 455 contacts were excluded from SARS-CoV-2 infection…”Said differently, exactly zero people were infected. The scientists, in typically understated fashion, offer up a comment about the question I hope you are asking yourself right now (namely, why are we all on lockdown if asymptomatic people with COVID-19 can’t spread the infection?), stating, “the result of this study may alleviate parts of the public concern about asymptomatic infected people.”
If this study had been published in early March, the odds that the world would have locked down are very, very low. Yet, this study, published only two weeks ago, is nowhere to be found in the media, and is never mentioned by policy makers. It just sits there, sharing the truth for anyone willing to listen.
Fact #4: Emerging science shows no spread of COVID-19 in the community (shopping, restaurants, barbers, etc.)
“There is no significant risk of catching the disease when you go shopping. Severe outbreaks of the infection were always a result of people being closer together over a longer period of time…”We just learned that asymptomatic people infected with COVID-19 are very unlikely to be able to spread the infection to others. Emerging and published science shows transmission of COVID-19 in retail establishments is extremely unlikely. Professor Hendrik Streeck from the University of Bonn is leading a study in Germany on the hard-hit region of Heinsberg and his conclusions, from laboratory work already completed, is very clear:
– Professor Hendrick Streek , University of Bonn

“There is no significant risk of catching the disease when you go shopping. Severe outbreaks of the infection were always a result of people being closer together over a longer period of time.Uh oh. You mean closing parks, closing stores, wearing gloves and masks at the grocery store, fumigating our groceries, and just being generally paranoid wasn’t necessary? As Dr. Streeck confirms:
“When we took samples from door handles, phones or toilets it has not been possible to cultivate the virus in the laboratory on the basis of these swabs….”
“It is important to obtain this data in order to make sure that decisions are taken based on facts rather than assumptions. The data should serve as a basis of information for the government so they can then think about their further course of action,” he said.And he continues:
“People could lose their jobs. They might not be able to pay their rent anymore and staying inside for a longer time can lead to weakening of our immune system.”And, finally:
“The goal is not a complete containment of the virus. We need to know where the actual capacity limits of our hospitals are. How many infections are too many? What do intensive care medics say?”
“It is important to start thinking about a ‘rollback’ strategy and his hope is to “deliver the relevant facts so that people have a good foundation for their decisions.”
Fact #5: Published science shows COVID-19 is NOT spread outdoors

“All identified outbreaks of three or more cases occurred in an indoor environment, which confirms that sharing indoor space is a major SARS-CoV-2 infection risk.”Said differently, there’s really no science to support all the outdoor bans that my home state of Oregon and so many other states have put in place. I’ll leave you with my favorite quote from the study because it’s really quite infuriating to read when you consider some of the ways Governors here in the U.S have behaved (and some still do) by banning all sorts of outdoor activities, arresting paddle boarders on the water, etc.:
“The transmission of respiratory infections such as SARS-CoV-2 from the infected to the susceptible is an indoor phenomenon.”Quick Update: Apparently the health minister of British Columbia, Canada, got the memo about the lack of airborne risk, this article appeared on June 1:

The article says:
One of B.C.’s top health officials, however, says medical professionals have a pretty clear picture of how the virus is transmitted. “There is absolutely no evidence that this disease is airborne, and we know that if it were airborne, then the measures that we took to control COVID-19 would not have worked,” Dr. Reka Gustafson, B.C.’s deputy provincial health officer, told CTV Morning Live Monday.”We are very confident that the majority of transmission of this virus is through the droplet and contact route….”The overwhelming majority of (COVID-19) transmissions occur through close, prolonged contact and that is not the pattern of transmission we see through airborne diseases,” she said.I sure hope Major League Baseball, the National Football League, and the NCAA are all paying attention…not to mention all the people in Portland here still riding bikes and running with masks on.
Fact #6: Science shows masks are ineffective to halt the spread of COVID-19, and The WHO recommends they should only be worn by healthy people if treating or living with someone with a COVID-19 infection
May 29th, the World Health Organization announced that masks should only be worn by healthy people if they are taking care of someone infected with COVID-19:“If you do not have any respiratory symptoms such as fever, cough or runny nose, you do not need to wear a mask,” Dr. April Baller, a public health specialist for the WHO, says in a video on the world health body’s website posted in March. “Masks should only be used by healthcare workers, caretakers or by people who are sick with symptoms of fever and cough.”Just before the COVID-19 madness, researchers in Hong Kong submitted a study for publication with the mouthful of a title, “Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures.” Oddly, the study, just published this month, is actually housed on the CDC’s own website, and directly contradicts recent advice from the CDC about wearing a mask. Namely, the study states:
“In our systematic review, we identified 10 RCTs that reported estimates of the effectiveness of face masks in reducing laboratory-confirmed influenza virus infections in the community from literature published during 1946–July 27, 2018….In pooled analysis, we found no significant reduction in influenza transmission with the use of face masks…Our systematic review found no significant effect of face masks on transmission of laboratory-confirmed influenza….Proper use of face masks is essential because improper use might increase the risk for transmission.”English translation: there is no evidence that wearing masks reduces the transmission of respiratory illnesses and, if masks are worn improperly (like when people re-use cloth masks), transmission could actually INCREASE. Moreover, this study was a meta-analysis, which means it dug deep into the archive of science (all the way back to 1946!) to reach its conclusions. Said differently, this is as comprehensive as science gets, and their conclusions were crystal clear: masks for the general population show no evidence of working to either slow the spread of respiratory viruses or protect people.
My favorite article is actually a review of much of the science and it’s a great place to start for anyone who likes to do their own research. Titled, “Why Face Masks Don’t Work: A Revealing Review”, it was written to challenge the need for dentists to wear face masks, but all the science quoted and conclusions drawn apply to airborne pathogens in any setting. Some of the best quotes:
“The science regarding the aerosol transmission of infectious diseases has, for years, been based on what is now appreciated to be ‘very outmoded research and an overly simplistic interpretation of the data.’ Modern studies are employing sensitive instruments and interpretative techniques to better understand the size and distribution of potentially infectious aerosol particles…The primary reason for mandating the wearing of face masks is to protect dental personnel from airborne pathogens. This review has established that face masks are incapable of providing such a level of protection.”And my favorite quote:
“It should be concluded from these and similar studies that the filter material of face masks does not retain or filter out viruses or other submicron particles. When this understanding is combined with the poor fit of masks, it is readily appreciated that neither the filter performance nor the facial fit characteristics of face masks qualify them as being devices which protect against respiratory infections. ”Here’s an article published in ResearchGate by noted Canadian physicist D.G. Rancourt, written directly in response to the COVID-19 outbreak, published last month. Titled, Masks Don’t Work: A review of science relevant to COVID-19 social policy.
“Masks and respirators do not work. There have been extensive randomized controlled trial (RCT) studies, and meta-analysis reviews of RCT studies, which all show that masks and respirators do not work to prevent respiratory influenza-like illnesses, or respiratory illnesses believed to be transmitted by droplets and aerosol particles. Furthermore, the relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective-dose is smaller than one aerosol particle.”To put this in simple terms: in order for a mask to really be effective that covered both your nose and mouth, you would asphyxiate. The minute the mask allows you to breathe, it can no longer filter the micro-particles that make you sick.
Finally, I often see this study from 2015 in the BMJ cited: “A cluster randomised trial of cloth masks compared with medical masks in healthcare workers“, and it bears repeating, since MOST of the masks I see people wearing in the community right now are cloth masks. Not only are these masks 100% ineffective at reducing the spread of COVID-19, but they can actually harm you. As the researchers explain:
“This study is the first RCT of cloth masks, and the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection. Further research is needed to inform the widespread use of cloth masks globally.”Increased risk of infection? Yes, that’s what it says. Other studies have also looked at the impact masks have on your oxygen levels (because you’re are forced to re-breathe your own Co2) and it’s not good. Scientists looked at oxygen levels of surgeons wearing masks while performing surgery and found: “Our study revealed a decrease in the oxygen saturation of arterial pulsations (SpO2) and a slight increase in pulse rates compared to preoperative values in all surgeon groups.”
 Just this past week, this article came out in the New England Journal of Medicine,
written my several doctors and public health officials with the title,
“Universal Masking in Hospitals in the Covid-19 Era,” and this statement
seems a perfect way to end my discussion of masks:
Just this past week, this article came out in the New England Journal of Medicine,
written my several doctors and public health officials with the title,
“Universal Masking in Hospitals in the Covid-19 Era,” and this statement
seems a perfect way to end my discussion of masks:We know that wearing a mask outside health care facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 30 minutes). The chance of catching Covid-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.
Fact #7: There’s no science to support the magic of a six-foot barrier

Where does the two-metre rule come from? Surprisingly, it can be traced back to research in the 1930s. Back then scientists established that droplets of liquid released by coughs or sneezes will either evaporate quickly in the air or be dragged by gravity down to the ground. And the majority of those droplets, they reckoned, would land within one to two metres. That is why it is said the greatest risks come from having the virus coughed at you from close range or from touching a surface – and then your face – that someone coughed onto. How conclusive is that?
Are you impressed with that science? Me neither. As this wonderful article explains:
A few early studies suggest that contaminated droplets could stay airborne for a few hours and pose a risk. But that research comes with a caveat: “While this research indicates that viral particles can be spread via bioaerosols, the authors stated that finding infectious virus has proven elusive and experiments are ongoing to determine viral activity in collected samples,” wrote Dr. Harvey Fineberg from the National Academies of Science, Engineering, and Medicine earlier this month.It goes further:
And the commonly held fear that a random passerby will infect a stranger? Here’s more grade-school level talk from the CDC: “COVID-19 is thought to spread mainly through close contact from person-to-person in respiratory droplets from someone who is infected. People who are infected often have symptoms of illness. Some people without symptoms may be able to spread the virus [which science from China has proven is untrue].”The article takes dead aim at so many Governors who are absolutely running with these completely unsupportable recommendations:
Not only would that sort of conclusion warrant a failing grade in any post-doctoral program, I am pretty sure the average eighth-grade science teacher would take a big red pen to that passage. “Thought.” “Some?” “May?” Keep in mind, there are no links to any scientific studies or papers for the average thinking person to review to decide whether those claims are legitimate.
The CDC also can’t quite make up its mind about the safety of large gatherings in the COVID-era. In mid-March, the agency asked Americans to limit gatherings of 250 people or more. A few weeks later, the White House, at the behest of the CDC, urged Americans to avoid gatherings of more than 10 people. There is no science, however, to support either number. (What is so fateful about 250 people? Why not 175? And why 10 people? Why not 16 or 17?)
Even that fuzzy advice has been bastardized by the petty tyrant lurking inside every big state governor, small-town mayor, and homeowners’ association president. Over the weekend, Michigan Governor Gretchen Whitmer banned people from going to a neighbor’s house. “All public and private gatherings of any size are prohibited,” Whitmer announced. “People can still leave the house for outdoor activities . . . recreational activities are still permitted as long as they’re taking place outside of six feet from anyone else.”…There will be plenty of soul-searching after this crisis abates: demanding to know the scientific rationale for keeping us six feet apart when people needed each other most should be at the top of the list.Recently, one of the top scientific advisors in the UK to Prime Minister Boris Johnson has made the same point, his statements covered in the Daily Mail last week in an article titled, Government scientific adviser says Britain’s two metre social distancing rule is unnecessary and based on ‘very fragile’ evidence. Professor Robert Dingwall stated:
‘I think it will be much harder to get compliance with some of the measures that really do not have an evidence base,’ he said. ‘I mean the two-metre rule was conjured up out of nowhere.’
When you digest all of the facts we now know about COVID-19, the simplest policy recommendation actually makes the most sense in my opinion: If you have COVID-19, stay home. If you must go out, wear a mask. Everyone else, wash your hands, and get on with your life. It should have been that easy, but instead we chose to lockdown society, an unprecedented step. Why?
Oh, and this is a real headline. God help us all.

“The Lockdowns Were the Black Swan”
Indeed, why did we lockdown society, and has it worked? I stole the phrase above from an opinion piece in the Wall Street Journal written by Editorial Board member Holman W. Jenkins, Jr., I believe he captured it perfectly:We started off sensibly. “This is not something [American families] generally need to worry about,” said CDC’s Dr. Nancy Messonnier in mid-January. “It’s a very, very low risk to the United States,” said Dr. Anthony Fauci a week later.Bill de Blasio, mayor of New York, urged residents to go about their business normally as recently as March 11.As coldblooded as it seems, these were the right statements at the time. Under “flatten the curve,” changes in public behavior aren’t needed until they are needed. Roll that around in your mind a bit. The better we do at equipping local hospitals, the less we need to bankrupt local businesses and their workers to slow the virus as it runs its course through society. That was the idea we started with. Not even the U.K. Imperial College study that so alarmed the world’s policy makers recommended indiscriminate lockdowns and shelter-in-place orders. If we meant what we said, we’ve overshot in many places. Beds are empty. A ventilator shortage did not materialize. We failed to set aside enough capacity to treat other medical conditions like strokes and heart attacks. This is costing lives.Why did we lockdown in the first place? Here are the facts.
What happened? From Bill Gates to your local editorialist, a new priority waddled to the fore. We decided that, whatever contributes to killing Americans at a routine total rate of 8,000 or so a day, it shouldn’t be the coronavirus.
Accidents, yes—6% of deaths. Heart disease, yes—23%. Flu and pneumonia, yes—2%.
These deaths are allowed but not deaths from the coronavirus even at the cost of economic ruin for millions. Of course the media and public are free to decide now they never wanted flatten the curve; they wanted to be spared the virus altogether. But explain how this is to be done. And explain why. The Economist magazine says we can’t restart the economy without an “unprecedented” $180 billion testing regime. Unprecedented is an interesting word because China, a country of 1.4 billion people with eight cities larger than New York, either must have developed such a system with nobody noticing or hasn’t found it necessary.
Fact #8: The idea of locking down an entire society had never been done and has no supportable science, only theoretical modeling

Dr. Henderson was convinced that it made no sense to force schools to close or public gatherings to stop. Teenagers would escape their homes to hang out at the mall. School lunch programs would close, and impoverished children would not have enough to eat. Hospital staffs would have a hard time going to work if their children were at home.
The measures embraced by Drs. Mecher and Hatchett would “result in significant disruption of the social functioning of communities and result in possibly serious economic problems,” Dr. Henderson wrote in his own academic paper responding to their ideas.
The answer, he insisted, was to tough it out: Let the pandemic spread, treat people who get sick and work quickly to develop a vaccine to prevent it from coming back.
Soon after, Dr. Henderson and several other prescient colleagues penned an important paper encapsulating many of these ideas, Disease Mitigation Measures in the Control of Pandemic Influenza, including this astonishing (given what just happened) conclusion:
There are no historical observations or scientific studies that support the confinement by quarantine of groups of possibly infected people for extended periods in order to slow the spread of influenza. A World Health Organization (WHO) Writing Group, after reviewing the literature and considering contemporary international experience, concluded that “forced isolation and quarantine are ineffective and impractical.”2 Despite this recommendation by experts, mandatory large-scale quarantine continues to be considered as an option by some authorities and government officials.35,43And they ended with a sentence so important I’m going to use really big font:
The interest in quarantine reflects the views and conditions prevalent more than 50 years ago, when much less was known about the epidemiology of infectious diseases and when there was far less international and domestic travel in a less densely populated world. It is difficult to identify circumstances in the past half-century when large-scale quarantine has been effectively used in the control of any disease.
If you’d like to read more about the origins of the lockdown idea and how it continued to circulate in public health circles, check out, “The 2006 Origins of the Lockdown Idea.” If you’d like to read more about Dr. D.A. Henderson, check out, “How a Free Society Deals with Pandemics, According to Legendary Epidemiologist and Smallpox Eradicator Donald Henderson.” Both articles are awesome and will make you sick to your stomach when you realize how many good scientists knew that a lockdown would be a disaster, and cost more lives than it could ever save.The negative consequences of large-scale quarantine are so extreme (forced confinement of sick people with the well; complete restriction of movement of large populations; difficulty in getting critical supplies, medicines, and food to people inside the quarantine zone) that this mitigation measure should be eliminated from serious consideration.
You’re likely equally shocked to see that as late as 2019, the World Health Organization DIDN’T EVEN LIST the idea of a total lockdown in their report titled “Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza.” Here’s their table of 18 possible non-pharmaceutical measures for countries to take in a pandemic, note all the things listed under the “Not recommended in any circumstances” row that are now happening every day!

Obvious question: if there was no science to support a lockdown and we’d never actually done one before and many in public health said it would be a terrible idea, why did it happen? There’s really two answers as best I can tell. The first answer is that the World Health Organization, early on in the pandemic, chose to praise the Chinese response of locking down Hubei Province, which effectively served to legitimize the practice, despite the extreme limitations of data available to anyone about the Chinese lockdown’s actual effectiveness. This article discusses the issue, and raises the question:
What changed the WHO’s mind and prompted it to praise the response of the Chinese authorities in Hubei province, which included the virtual incarceration of 60 million people? It was this, more than anything else, that persuaded governments across the world to lockdown their citizens.
The second answer is that newly-created disease models scared the living daylights out of world leaders, and the modelers stood ready to offer a simple solution to their made-up numbers: lock everything down, NOW!
Fact #9: The epidemic models of COVID-19 have been disastrously wrong, and both the people and the practice of modeling has a terrible history
While many disease models have been used during the COVID-19 pandemic, two have been particularly influential in the public policy of lockdowns: Imperial College (UK) and the IHME (Washington, USA). They’ve both proven to be unmitigated disasters.Imperial College: It’s safe to say that the reason the United States locked down, and the reason the White House extended their lockdowns was almost exclusively due to the models created by Imperial College Professor Neil Ferguson. As the Washington Post explained:
Officials have said the Imperial College’s eye-popping 2.2 million death projection convinced Trump to stop dismissing the outbreak and take it more seriously. Similarly, officials said, the new projection of 100,000 to 240,000 deaths is what convinced Trump to extend restrictions for 30 days and abandon his push to reopen parts of the country by Easter, which many health experts believe could have worsened the outbreak.Oddly, Professor Ferguson has a history of massive overestimation of pandemics, but apparently no one bothered to consider that in taking his advice. The Spectator spelled out his incredibly bad calls on three previous emerging diseases (he actually has more terrible calls, I’m just highlighting three):
2002, Mad Cow Disease:
In 2002, Ferguson predicted that between 50 and 50,000 people would likely die from exposure to BSE (mad cow disease) in beef. He also predicted that number could rise to 150,000 if there was a sheep epidemic as well. In the UK, there have only been 177 deaths from BSE.
2005, Bird Flu:
In 2005, Ferguson said that up to 200 million people could be killed from bird flu. He told the Guardian that ‘around 40 million people died in 1918 Spanish flu outbreak… There are six times more people on the planet now so you could scale it up to around 200 million people probably.’ In the end, only 282 people died worldwide from the disease between 2003 and 2009.
2009, Swine Flu:
In 2009, Ferguson and his Imperial team predicted that swine flu had a case fatality rate 0.3 per cent to 1.5 per cent. His most likely estimate was that the mortality rate was 0.4 per cent. A government estimate, based on Ferguson’s advice, said a ‘reasonable worst-case scenario’ was that the disease would lead to 65,000 UK deaths. In the end swine flu killed 457 people in the UK and had a death rate of just 0.026 per cent in those infected.
I don’t know, don’t you think that history should have mattered more before relying on his model to lock down our entire country? It actually gets worse. From the National Review:
Johan Giesecke, the former chief scientist for the European Center for Disease Control and Prevention, has called Ferguson’s model “the most influential scientific paper” in memory. He also says it was, sadly, “one of the most wrong.”
And more:
Jay Schnitzer, an expert in vascular biology and a former scientific direct of the Sidney Kimmel Cancer Center in San Diego, tells me: “I’m normally reluctant to say this about a scientist, but he dances on the edge of being a publicity-seeking charlatan.”
One simple example of how wrong the Imperial College model was would be Sweden, here’s the details:
Indeed, Ferguson’s Imperial College model has been proven wildly inaccurate. To cite just one example, it saw Sweden paying a huge price for no lockdown, with 40,000 COVID deaths by May 1, and 100,000 by June. Sweden now has 2,854 deaths and peaked two weeks ago. As Fraser Nelson, editor of Britain’s Spectator, notes: “Imperial College’s model is wrong by an order of magnitude.”And, finally:
Indeed, Ferguson has been wrong so often that some of his fellow modelers call him “The Master of Disaster.”Oh, and Professor Ferguson recently resigned from his position because he broke lockdown curfew…to have an affair with a married woman. I’ll end with a quote from the man who I believe will emerge as the biggest hero of this whole mess, Sweden’s Anders Tegnell, the man who chose not to lock his country down:
One person who’s skeptical of Professor Ferguson’s modeling is Anders Tegnell, the epidemiologist who’s been advising the Swedish Government. “It’s not a peer-reviewed paper,” he said, referring to the Imperial College March 16th paper. “It might be right, but it might also be terribly wrong. In Sweden, we are a bit surprised that it’s had such an impact.”IHME: If the Imperial College model was really the motivation for both President Trump, Boris Johnson, and then many other world leaders to lockdown, the IHME models have almost always been the “science” state Governors cite to demonstrate how many lives their lockdowns are saving. It’s a nice gig, really. Find a model that massively overestimates the deaths in your state, lock it down, and then have the modelers show you how many lives you have saved. Luckily, other scientists have been watching, and the IHME model has received one of the most ferocious beat-downs I have ever seen in the scientific literature from Professors at the University of Sydney, Northwestern, and UTEP. Titled, Learning as We Go – An Examination of the Statistical Accuracy of COVID-19 Daily Death Count Predictions and released last week, the study effectively says that the IHME model is dangerously inaccurate, but in a somewhat cordial, scientific way. The authors write:
Specifically, the true number of next day deaths fell outside the IHME prediction intervals as much as 76% of the time, in comparison to the expected value of 5%. Regarding the updated models, our analyses indicate that the April models show little, if any, improvement in the accuracy of the point estimate predictions.And then they land the big punch:
Our analysis calls into question the usefulness of the predictions to drive policy making and resource allocation.In English: the IHME models are so bad at forecasting they shouldn’t be relied upon for anything. Need more? National Review’s Andrew McCarthy was very eloquent all the way back on April 9th in criticizing the IMHE models’ inaccuracy and uselessness:
The model on which the government is relying is simply unreliable. It is not that social distancing has changed the equation; it is that the equation’s fundamental assumptions are so dead wrong, they cannot remain reasonably stable for just 72 hours. And mind you, when we observe that the government is relying on the models, we mean reliance for the purpose of making policy, including the policy of completely closing down American businesses and attempting to confine people to their homes because, it is said, no lesser measures will do.”And how does Mr. McCarthy, a senior fellow at the National Review Institute, think these models have performed?
“To describe as stunning the collapse of a key model the government has used to alarm the nation about the catastrophic threat of the coronavirus would not do this development justice.”My own Governor here in Oregon, Kate Brown, is fond of invoking the phrase that she is “following the science.” Recently, a Circuit Court overturned her lockdown order after a lawsuit was filed from a number of churches. Governor Brown released this statement:
From the beginning of this crisis, I have worked within my authority, using science and data as my guide, heeding the advice of medical experts. This strategy has saved lives and protected Oregonians from the worst of the COVID-19 pandemic.What “science” is Governor Brown relying upon? The IHME model. Still think that’s “science”?
Finally, Michael Fumento wrote an excellent article arguing that “After Repeated Failures, It’s Time To Permanently Dump Epidemic Models.” As he explains:
The models essentially have three purposes: 1) To satisfy the public’s need for a number, any number; 2) To bring media attention for the modeler; and 3) To scare the crap out of people to get them to “do the right thing.” That can be defined as “flattening the curve” so health care systems aren’t overridden, or encouraging people to become sheeple and accept restrictions on liberties never even imposed during wars. Like Ferguson, all the modelers know that no matter what the low end, headlines will always reflect the high end. Assuming it’s possible to model an epidemic at all, any that the mainstream press relays will have been designed to promote panic.Opinion #2: Roger Koppl, inside the mind of a disease modeler
 I just thought this was such a great description of the human side of being a disease forecaster, written by Professor of Finance Roger Koppl from Syracuse:
I just thought this was such a great description of the human side of being a disease forecaster, written by Professor of Finance Roger Koppl from Syracuse:Think if it were you. You’re an epidemiologist and the prime minister calls to ask you how many will die if we don’t have a lockdown. What do you tell him? You can’t just look up the number. The pandemic is only now taking off and your knowledge of it is correspondingly sketchy. It’s hard to say. Every number is a guess. If you give the prime minister a low number, there will be no lockdown. What if he accepts your low number and we have no lockdown? Maybe everything will be fine. But maybe there will be many more deaths than you predicted. You will get blamed. People will shame you as a bad scientist. And, because you are a good and decent person, you will feel guilty. Blame, shame, and guilt. This is a bad outcome.Makes sense, and I think most American Governors who locked down are running with this: the model said we’d have X number of deaths. Now the model says the lockdown ensured a fraction of X deaths—I’m your savior!
If you give him a high number, there will be lockdown. No one will ever be able to say that your estimate was too high, because your estimate assumed no lockdown. Even if a lot of people die during the lockdown you can say, “See? Think how much worse it would have been without the lockdown.” Thus, if you give the prime minister a high number, you will get credit for saving lives. You will be able to take pride in your sterling reputation as a scientist. And you won’t have to feel guilty about lost lives. Praise, pride, and innocence. This is a good outcome. The logic of the situation is clear. You have every incentive to predict doom and gloom if no lockdown is ordered.
Fact #10: The data shows that lockdowns have NOT had an impact on the course of the disease.
This is certainly the fact that people will have the hardest time with: who wants to believe that all this suffering and isolation was for no reason? But, there are more than enough states and countries that didn’t lockdown, or locked down for a much shorter time, or in a much different manner, to provide plenty of data. Perhaps the simplest explanation for why lockdowns have been ineffective is the easiest: COVID-19 was in wide circulation much EARLIER than experts thought. This alone would explain why lockdowns have been so ineffective, but whatever the final explanation, let’s see what the data says.I’m going to start with a source that you might consider unusual, the global bank JP Morgan. Of all the facts I have covered, this one about the ineffectiveness of lockdowns has become the most politicized, because it’s being used to begin playing the blame game. JP Morgan, on the other hand, creates their analysis to do something very nonpartisan: make money. Their analysts crunch data to see which economies are likely to restart first, and you shouldn’t be surprised at this point to discover three things: 1) the least damaged economies are the ones that did the lest onerous lockdowns, 2) lifting lockdowns has had no negative impact on deaths or hospitalizations, and 3) lifting lockdowns had not increased viral transmission. Reading the JP Morgan conclusions is profoundly depressing, because here in the U.S. many communities are STILL being put through many different lockdown mandates, despite overwhelming evidence to their ineffectiveness. Consider this chart from JP Morgan that shows “that many countries saw their infection rates fall rather than rise again when they ended their lockdowns – suggesting that the virus may have its own ‘dynamics’ which are ‘unrelated’ to the emergency measures.”

JP Morgan strategist and paper author Marko Kolanovic is another one of my heroes, because, well, he says everything I wish many other people were saying, consider this quote:
“Unlike rigorous testing of new drugs, lockdowns were administered with little consideration that they might not only cause economic devastation but potentially more deaths than Covid-19 itself.”Kolanovic and his team also show that transmissibility of the virus has actually DECREASED after lockdowns have been lifted in U.S. states, through the measurement known as “RO”. As the Daily Mail explains, “many states saw a lower rate of transmission (R) after full-scale lockdowns were ended.”

TJ Rogers, the founder of Cypress Semiconductor, and a team of his engineers also analyzed the data, and published their results in this piece in the Wall Street Journal titled “Do Lockdowns Save Many Lives? In Most Places, the Data Say No.” They explain:
We ran a simple one-variable correlation of deaths per million and days to shutdown, which ranged from minus-10 days (some states shut down before any sign of Covid-19) to 35 days for South Dakota, one of seven states with limited or no shutdown. The correlation coefficient was 5.5%—so low that the engineers I used to employ would have summarized it as “no correlation” and moved on to find the real cause of the problem.Translation: something other than lockdowns must explain the course of the virus (see Fact #14). Thomas A. J. Meunier of the Woods Hole Oceanographic Institution released this report in early May titled “Full lockdown policies in Western Europe countries have no evident impacts on the COVID-19 epidemic.” Like JP Morgan’s report, his conclusion is depressing:
Our results show a general decay trend in the growth rates and reproduction numbers two to three weeks before the full lockdown policies would be expected to have visible effects. Comparison of pre and post lockdown observations reveals a counter-intuitive slowdown in the decay of the epidemic after lockdown.And, the clincher:
Estimates of daily and total deaths numbers using pre-lockdown trends suggest that no lives were saved by this strategy, in comparison with pre-lockdown, less restrictive, social distancing policies.Bloomberg’s Elain He and colleagues also analyzed the data in this article titled, “The Results of Europe’s Lockdown Experiment Are In.” Their conclusion is unlikely to surprise you:
But, as our next chart shows, there’s little correlation between the severity of a nation’s restrictions and whether it managed to curb excess fatalities — a measure that looks at the overall number of deaths compared with normal trends.Speaking of Europe, we should all thank God for Sweden. By choosing NOT to lockdown, the Swedes have proven that society can survive without a strict lockdown, and hopefully their results will prevent lockdowns from ever happening again. If you have followed this story closely, you know that naysayers were predicting doom for Sweden (and for Florida and Georgia, more on them in a moment), and none of that has ever come to pass. Conveniently, the World Health Organization went from praising the response of the Chinese lockdown in Wuhan—which likely ignited the lockdown mania—to holding up Sweden as the model for how to combat an epidemic. (Read: “WHO reverses course, praises lockdown-ignoring Sweden”.)
Fact #11: Florida locked down late, opened early, and is doing fine, despite predictions of doom
The best article I have read about Florida’s Governor Ron DeSantis comes from this one on the National Review on May 20th. I was pleasantly surprised by what a rational student of history Governor Desantis was, as he explains:“One of the things that bothered me throughout this whole time was, I researched the 1918 pandemic, ’57, ’68, and there were some mitigation efforts done in May 1918, but never just a national-shutdown type deal. There was really no observed experience about what the negative impacts would be on that.”Unlike many of his peers, Governor Desantis found doomsday models to be unhelpful:
The DeSantis team also didn’t put much stock in dire projections. “We kind of lost confidence very early on in models,” a Florida health official says. “We look at them closely, but how can you rely on something when it says you’re peaking in a week and then the next day you’ve already peaked?” Instead, “we started really focusing on just what we saw.”Instead, they took a rifle shot approach on the citizens most at-risk: nursing home residents, of which Florida has the most in the nation:
Inspectors and assessment teams visited nursing homes. The state homed in on facilities where, Mayhew says, “we had historically cited around infection control. We used that to prioritize our visits to those facilities, understanding that the guidance from CDC was changing frequently. So our initial focus was to be an effective resource education to provide guidance to these facilities to make sure they understood how to request personal protective equipment from the state.”Which brings us to New York, the state that every other Governor who locked their people down points to, and says something to the effect of, “by locking down early, we avoided being New York.” Is that really true?
Florida, DeSantis notes, “required all staff and any worker that entered to be screened for COVID illness, temperature checks. Anybody that’s symptomatic would just simply not be allowed to go in.” And it required staff to wear PPE. “We put our money where our mouth is,” he continues. “We recognized that a lot of these facilities were just not prepared to deal with something like this. So we ended up sending a total of 10 million masks just to our long-term-care facilities, a million gloves, half a million face shields.”
Florida fortified the hospitals with PPE, too, but DeSantis realized that it wouldn’t do the hospitals any good if infection in the nursing homes ran out of control : “If I can send PPE to the nursing homes, and they can prevent an outbreak there, that’s going to do more to lower the burden on hospitals than me just sending them another 500,000 N95 masks.”
It’s impossible to overstate the importance of this insight, and how much it drove Florida’s approach, counter to the policies of New York and other states. (“I don’t want to cast aspersions on others, but it is incredible to me, it’s shocking,” says the Florida health official, “that Governor Cuomo [and others] are able to kind of just avoid real questions about their policies early on to actually send individuals into the nursing home, which is completely counter to the real data.”)
(Special note: there are MANY other states—and countries—with data similar to Florida’s, including Georgia, Texas, Arkansas, Utah, Japan, and of course, Sweden, to name just a few. In ALL cases, the media predicted doom, and even President Trump criticized Georgia’s early opening by their courageous Governor Brian Kemp, and Georgia’s numbers today look great.)
Fact #12: New York’s above average death rate appears to be driven by a fatal policy error combined with aggressive intubations.
Forbes recently published an article explaining just how concentrated COVID-19 deaths really are in a single population, titled “The Most Important Coronavirus Statistic: 42% Of U.S. Deaths Are From 0.6% Of The Population,” the article explains:2.1 million Americans, representing 0.62% of the U.S. population, reside in nursing homes and assisted living facilities…According to an analysis that Gregg Girvan and I conducted for the Foundation for Research on Equal Opportunity, as of May 22, in the 43 states that currently report such figures, an astounding 42% of all COVID-19 deaths have taken place in nursing homes and assisted living facilities.Forbes also points out that the risk coronavirus-type illnesses represent to nursing home populations is nothing new:
The tragedy is that it didn’t have to be this way. On March 17, as the pandemic was just beginning to accelerate, Stanford epidemiologist John Ioannidis warned that “even some so-called mild or common-cold-type coronaviruses have been known for decades [to] have case fatality rates as high as 8% when they infect people in nursing homes.” Ioannidis was ignored.In his recent meta-analysis on the real Infection Fatality Rate of COVID-19, Dr. Ioannidis explained the policy error in New York that likely contributed to thousands of preventable deaths:
Massive deaths of elderly individuals in nursing homes, nosocomial infections, and overwhelmed hospitals may also explain the very high fatality seen in specific locations in Northern Italy and in New York and New Jersey. A very unfortunate decision of the governors in New York and New Jersey was to have COVID-19 patients sent to nursing homes.Dr. Ioannidis also mentions the choice by medical personnel in New York to quickly put patients on ventilators, which doctors now realize likely does more harm than good (Read: 80% of NYC’s coronavirus patients who are put on ventilators ultimately die, and some doctors are trying to stop using them.):
Use of unnecessarily aggressive management (e.g. mechanical ventilation) may also have contributed to worse outcomes.
The New York Post was particularly harsh in criticizing New York’s nursing home policy:
The carnage started in March, when hospitals inundated with COVID-19 patients insisted on clearing out elderly patients, even if they were still infected, and sending them to whatever nursing homes had empty beds. To swing that, they had to get rid of a safety regulation requiring patients to test negative twice for COVID-19 before being placed in a home. The state Health Department willingly complied.When your Governor tries to tell you that their destructive decision to lock everyone down saved you from being New York, remember Florida and Sweden. Oh, and don’t forget the country no doomsday folks want to even discuss: Japan:
On March 25, Gov. Cuomo’s Health Department mandated that nursing homes had to accept COVID patients and barred requiring any COVID tests for admission. Facilities like Newfane had to fly blind, not knowing which incoming patients had it.
The American Health Care Association called it a “recipe for disaster.” The Committee to Reduce Infection Deaths urged Cuomo to change course…Bottom line: 11,000 to 12,000 nursing-home and assisted-living residents have died from COVID-19, half of all the virus deaths statewide…That awful death toll didn’t have to happen. It’s six times the number of nursing-home fatalities as in Florida or California, both more populous states.
Japan yesterday [May 25th] declared at least a temporary victory in its battle with COVID-19, and it triumphed by following its own playbook. It drove down the number of daily new cases to near target levels of 0.5 per 100,000 people with voluntary and not very restrictive social distancing and without large-scale testing…The dwindling numbers of new cases led the government to start to lift the state of emergency for much of Japan on 14 May, ahead of the intended 31 May schedule. Yesterday’s announcement completed the lift, relieving Tokyo and four other prefectures.
Fact #13: Public health officials and disease epidemiologists do NOT consider the other negative societal consequences of lockdowns
If you asked me for how a suggestion for how to lose a few pounds and I said, “Stop eating or drinking anything,” would you take my advice? It would work to achieve your goals, but you may not like the side effects. That’s basically what has happened here. Rather than being ONE input on policy, public health officials were handed the keys to the convertible without their license, and off they sped! Look what Dr. Anthony Fauci said to Congress earlier this month:I’m a scientist, a physician, and a public health official. I give advice, according to the best scientific evidence. There are a number of other people who come into that and give advice that are more related to the things that you spoke about, the need to get the country back open again, and economically. I don’t give advice about economic things. I don’t give advice about anything other than public health.The Wall Street Journal actively criticized this single-dimensional thinking by American public health officials, noting, “Dr. Fauci is clear on the fact that Americans should not rely on him to conduct cost-benefit analysis of the policies he is recommending.” This excellent critique of the Imperial College model makes a similar point: “The Imperial College paper is a one-sided analysis. It looks at the benefits of a lockdown without going into the costs.”
So wait, all these models that predicted doom from COVID-19 didn’t consider deaths caused by the lockdowns from suicide, skipped doctors appointments, and unemployment? So who should be making these complex policy decisions? At least in the United States, I hold 51 people responsible: the President and 50 state Governors. And, if you expect any of them to issue a mea culpa for a terrible decision, don’t hold your breath, from the Issues & Insights Editorial Board:
Don’t expect anyone to admit they were wrong. The public health community – which has been peddling wildly exaggerated predictions of deaths – will never do so. Nor will Democrats and the press – which are committed to the narrative that every death in the U.S. is President Donald Trump’s fault. Trump isn’t likely to, either, since he agreed to shutting down the economy after he started taking his cues from public health doomsayers.Opinion #3: Yoram Lass, former director of Israel’s Health Ministry
 Unlike
American public health officials, who seem wed to the idea of
preventing COVID-19 no matter what the cost, I have been heartened to
see public health officials in other countries with a much more complete
understanding of the TOTAL cost to society than any public health
decision causes. And of all the international straight-talking public
health officials, no one puts it any more directly than my favorite:
Yoram Lass of Israel. In this excellent interview with Spiked Online—which you should really read in full—Dr. Lass offers up the following nugget:
Unlike
American public health officials, who seem wed to the idea of
preventing COVID-19 no matter what the cost, I have been heartened to
see public health officials in other countries with a much more complete
understanding of the TOTAL cost to society than any public health
decision causes. And of all the international straight-talking public
health officials, no one puts it any more directly than my favorite:
Yoram Lass of Israel. In this excellent interview with Spiked Online—which you should really read in full—Dr. Lass offers up the following nugget:It is the first epidemic in history which is accompanied by another epidemic – the virus of the social networks. These new media have brainwashed entire populations. What you get is fear and anxiety, and an inability to look at real data. And therefore you have all the ingredients for monstrous hysteria….Compared to that rise, the draconian measures are of biblical proportions. Hundreds of millions of people are suffering. In developing countries many will die from starvation. In developed countries many will die from unemployment. Unemployment Is mortality. More people will die from the measures than from the virus. And the people who die from the measures are the breadwinners. They are younger. Among the people who die from coronavirus, the median age is often higher than the life expectancy of the population. What has been done is not proportionate. But people are afraid. People are brainwashed. They do not listen to the data. And that includes governments.
Fact #14: There is a predictive model for the viral arc of COVID-19, it’s called Farr’s Law, and it was discovered over 100 years ago
Dr. Lass, in his interview highlighted above, also made a point that we already knew, long before the lockdowns, how COVID-19 was likely to behave because, well, we’ve been dealing with new viruses since the dawn of man:If you look at the coronavirus wave on a graph, you will see that it looks like a spike. Coronavirus comes very fast, but it also goes away very fast. The influenza wave is shallow as it takes three months to pass, but coronavirus takes one month.That ALL viruses follow a natural bell curve, with slopes roughly equal on the way up and down, was discovered by Dr. William Farr more than 100 years ago, and it’s known as Farr’s law. Recently, Chinese and American scientists published a study to see if COVID-19 would behave according to Farr’s law, and here’s the chart from their recent paper:

As you can see, the predicted path of the virus in China (orange dotted line) and the actual path of the virus (blue dotted line) are a match. This paper, created all the way back on February 8th, could have saved policy-makers much heartache. A renowned Israeli scientist made this same point about the natural arc of the virus more than a month ago, in the middle of Israel’s lockdown:
A prominent Israeli mathematician, analyst and former general claims simple statistical analysis demonstrates that the spread of COVID-19 peaks after about 40 days and declines to almost zero after 70 days — no matter where it strikes, and no matter what measures governments impose to try to thwart it.(Dr. Ben-Israell, FYI, is arguably Israel’s most famous scientist, read his resume for yourself.) I put the Farr’s law idea to the test with the local data I have here in Oregon, and what you can clearly see is that COVID-19 was ALREADY following a natural, expected viral arc BEFORE our Governor Kate Brown imposed a lockdown. (Note: Lockdown order issued on March 23rd, it would take 2 weeks to see a positive impact on hospitalization numbers, but the virus was already on the decline, much as both Dr. Lass and Dr. Ben-Israel predicted.)
Prof Isaac Ben-Israel, head of the Security Studies program in Tel Aviv University and the chairman of the National Council for Research and Development, told Israel’s Channel 12 (Hebrew) Monday night that research he conducted with a fellow professor, analyzing the growth and decline of new cases in countries around the world, showed repeatedly that “there’s a set pattern” and “the numbers speak for themselves.”
While he said he supports social distancing, the widespread shuttering of economies worldwide constitutes a demonstrable error in light of those statistics. In Israel’s case, he noted, about 140 people normally die every day. To have shuttered much of the economy because of a virus that is killing one or two a day is a radical error that is unnecessarily costing Israel 20% of its GDP, he charged.

I really enjoyed this explanation of Farr’s law by Michael Fumento:
The only “model” with any success is actually quite accomplished and appeared in 1840, when a “computer” was an abacus. It’s called Farr’s Law, and is actually more of an observation that epidemics grow fastest at first and then slow to a peak, then decline in a more-or-less symmetrical pattern. As you might guess from the date, it precedes public health services and doesn’t require lockdowns or really any interventions at all. Rather, the disease grabs the low-hanging fruit (with COVID-19 that’s the elderly with co-morbid conditions) and finds it progressively harder to get more fruit.
Fact #15: The lockdowns will cause more death and destruction than COVID-19 ever did
My final fact is the most depressing. Of course, it’s impossible today to find all the data to show how destructive unnecessary lockdowns have been, but many people are already trying. Economically, the costs to the United States will be measure in the multi-trillions. It didn’t have to be this way, Sweden just reported that GDP grew in their first quarter!I’ll highlight a number of different takes so you get the basic picture, and it’s really ugly. Last week, writing in The Hill, a group of professors from Stanford, Duke, University of Chicago, and Hebrew University penned a sobering piece titled, The COVID-19 shutdown will cost Americans millions of years of life, where they explained:
Although well-intentioned, the lockdown was imposed without consideration of its consequences beyond those directly from the pandemic…The policies have created the greatest global economic disruption in history, with trillions of dollars of lost economic output. These financial losses have been falsely portrayed as purely economic. To the contrary, using numerous National Institutes of Health Public Access publications, Centers for Disease Control and Prevention (CDC) and Bureau of Labor Statistics data, and various actuarial tables, we calculate that these policies will cause devastating non-economic consequences that will total millions of accumulated years of life lost in the United States, far beyond what the virus itself has caused…Considering only the losses of life from missed health care and unemployment due solely to the lockdown policy, we conservatively estimate that the national lockdown is responsible for at least 700,000 lost years of life every month, or about 1.5 million so far — already far surpassing the COVID-19 total.One of the lead authors of the study, the aforementioned Dr. Scott Atlas, went on Fox News to further explain the results of their analysis:
“I think one thing that’s not somehow receiving attention is the CDC just came out with their fatality rates,” Atlas said. “And lo and behold, they verify what people have been saying for over a month now, including my Stanford epidemiology colleagues and everyone else in the world who’s done this analysis — and that is that the infection fatality rate is less than one-tenth of the original estimate. The policy itself is killing people. I mean, I think everyone’s heard about 650,000 people on cancer, chemo, half of whom didn’t come in. Two thirds of cancer screenings didn’t come in. 40 percent of stroke patients urgently needing care didn’t come in,” Atlas said.Remember how the lockdown was supposed to keep hospitals open to manage a surge of patients? Well, now the healthcare system is facing disaster: Doctors face pay cuts, furloughs and supply shortages as coronavirus pushes primary care to the brink CNBC reports:
Stanford’s Dr. John Ioaniddis penned an excellent article for the Boston Review, spelling out the catastrophic impact the lockdown is having on healthcare:It’s not just doctors’ offices in New York, the epicenter of the coronavirus epidemic in the U.S., that are experiencing financial hardship. Some 51% of primary-care providers are uncertain about their financial future over the next four weeks, and 42% have either laid off or furloughed staff, according to a survey of 2,700 practices across the U.S. by the nonprofit Primary Care Collaborative and Larry A. Green Center. In addition, 13% predict closure within the next month.
 At
the same time, we should not look away from the real harms of the most
drastic of our interventions, which also disproportionately affect the
disadvantaged. We know that prolonged lockdown of the entire population
has delayed cancer treatments and has made people with serious disease like heart attacks avoid going to the hospital. It is leading hospital systems to furlough and lay off personnel, it is devastating mental health, it is increasing domestic violence and child abuse,
and it has added at least 36.5 million new people to the ranks of the
unemployed in the United States alone. Many of these people will lose
health insurance, putting them at further risk of declining health and
economic distress. Prolonged unemployment is estimated to lead to an
extra 75,000 deaths of despair in the United States alone over the coming decade. At a global level, disruption has increased the number of people at risk of starvation to more than a billion, suspension of mass vaccination campaigns is posing a threat of resurgence of infectious diseases that kill children, modeling suggests an excess of 1.4 million deaths from tuberculosis by 2025, and a doubling of the death toll from malaria in
2020 is expected compared with 2018. I hope these modeling predictions
turn out to be as wrong as several COVID-19 modeling predictions have,
but they may not. All of these impacts matter, too. Policymakers must
consider the harms of restrictive policies, not just their benefits.
At
the same time, we should not look away from the real harms of the most
drastic of our interventions, which also disproportionately affect the
disadvantaged. We know that prolonged lockdown of the entire population
has delayed cancer treatments and has made people with serious disease like heart attacks avoid going to the hospital. It is leading hospital systems to furlough and lay off personnel, it is devastating mental health, it is increasing domestic violence and child abuse,
and it has added at least 36.5 million new people to the ranks of the
unemployed in the United States alone. Many of these people will lose
health insurance, putting them at further risk of declining health and
economic distress. Prolonged unemployment is estimated to lead to an
extra 75,000 deaths of despair in the United States alone over the coming decade. At a global level, disruption has increased the number of people at risk of starvation to more than a billion, suspension of mass vaccination campaigns is posing a threat of resurgence of infectious diseases that kill children, modeling suggests an excess of 1.4 million deaths from tuberculosis by 2025, and a doubling of the death toll from malaria in
2020 is expected compared with 2018. I hope these modeling predictions
turn out to be as wrong as several COVID-19 modeling predictions have,
but they may not. All of these impacts matter, too. Policymakers must
consider the harms of restrictive policies, not just their benefits.Heck, more than 600 doctors recently appealed to President Trump to lift the lockdowns, according to Forbes:

More than 600 of the nation’s physicians sent a letter to President Trump this week calling the coronavirus shutdowns a “mass casualty incident” with “exponentially growing negative health consequences” to millions of non COVID patients.
“The downstream health effects…are being massively under-estimated and under-reported. This is an order of magnitude error,” according to the letter initiated by Simone Gold, M.D., an emergency medicine specialist in Los Angeles.It’s no surprise that suicides are on the rise in localities that locked down, and that prescriptions for sleep and anti-anxiety medications have skyrocketed. And it was just reported that, “Social isolation can increase a person’s risk of dying early by up to 50 per cent, a new study has suggested.” Even Dr. Fauci, arguably the lockdown’s most enthusiastic supporter, has gotten religion recently, as CNBC reported:
Stay-at-home orders intended to curb the spread of the coronavirus could end up causing “irreparable damage” if imposed for too long, White House health advisor Dr. Anthony Fauci told CNBC on Friday.Dr. Fauci, you are very, very late to the party. In fact, one of my biggest issues with this entire mess, is how Dr. Fauci and others like him have done almost NOTHING to educate the American public about the new science and information we now have about COVID-19, which would have not only meaningfully reduced panic but also perhaps given Governors more support to re-open more quickly…
“I don’t want people to think that any of us feel that staying locked down for a prolonged period of time is the way to go,” Fauci said during an interview with CNBC’s Meg Tirrell on “Halftime Report.”
Fact #16: All these phased re-openings are utter nonsense with no science to support them, but they will all be declared a success
I found this Wall Street Journal article about Washington’s Governor Jay Inslee to be particularly telling:Mr. Inslee’s “Covid-19 dashboard,” which is supposed to provide a science-based path for Washington’s recovery, is much the same story. The online dashboard includes “dials” for five public-safety variables but gives no indication of how each is calculated or where the dials need to be to begin the various phases of reopening. When will builders be allowed to start new construction? When will small stores be able to open like Home Depot is open? The dashboard is designed to imply science but lacks meaningful data.Yup, still waiting for your Phase 1 or Phase 2 re-opening? Trust me, whomever conjured up your state’s plan is quite literally making things up as they go along. And, given the extreme range of plans taking place—even in neighboring counties—the odds that they have ANYTHING to do with the arc of the virus is exactly ZERO, but you already knew that if you read this far. The good news is they will ALL succeed, because we never needed to lockdown in the first place—MISSION ACCOMPLISHED.
(It’s interesting to look back to early May at the headlines where public health officials predicted disaster for Florida—Miami Herald: How safe is Florida’s reopening plan? Public health experts give a candid critique—are other Governor’s ever going to think for themselves the way Ron DeSantis did?)
How the hell did we get here?
This week, I was really struck by this headline from the Foundation for Economic Education:
As Sweden’s top infectious disease expert recently explained, Sweden’s approach to the pandemic is more orthodox than the current lockdown approach, at least compared to historical standards.Stanford’s Dr. Scott Atlas is, IMO, one of the true heroes of this quagmire, and I found his essay about the lack of leadership by American public health officials during this crisis to be one of his best. While the public health officials have done a great job scaring the daylights out of Americans, they’ve done very little to update Americans on the emerging science that has proved many of our initial fears to be unsupported by science. We still have MILLIONS of Americans who are scared to leave their home, and my guess is that many think COVID-19’s IFR is closer to smallpox (30%) than to the seasonal flu. As Dr. Atlas wrote on May 3rd in The Hill:
“Are the people closing society completely, which has really never been done before, more or less orthodox than Sweden?” Anders Tegnell asked recently. “[Sweden is doing] what we usually do in public health: giving lots of responsibility to the population, trying to achieve a good dialogue with the population, and achieve good results with that.”
Tegnell’s point deserves attention. While nations today appear comfortable instituting mass lockdowns to prevent the spread of a deadly respiratory virus, the practice appears to be unprecedented.
The basis of reassuring the public about re-entry is repeating the facts about the threat and who it targets. By now, studies from Europe and the U.S. all suggest that the overall fatality rate is far lower than early estimates. And we know who to protect, because this disease – by the evidence – is not equally dangerous across the population. In Michigan’s Oakland County, 75 percent of deaths were in those over 70 years old; 91 percent were in people over 60, similar to what was noted in New York. And younger, healthier people have virtually zero risk of death and little risk of serious disease; as I have noted before, under one percent of New York City’s hospitalizations have been patients under 18 years of age, and less than one percent of deaths at any age are in the absence of underlying conditions.I still struggle to make sense of how the hell we got here. I think one of the best essays you will ever read on this topic is a 2-part series written by bioengineer Yinon Weiss:
Part 1: How Fear, Groupthink Drove Unnecessary Global Lockdowns. Excerpt:
In the face of a novel virus threat, China clamped down on its citizens. Academics used faulty information to build faulty models. Leaders relied on these faulty models. Dissenting views were suppressed. The media flamed fears and the world panicked. That is the story of what may eventually be known as one of the biggest medical and economic blunders of all time. The collective failure of every Western nation, except one, to question groupthink will surely be studied by economists, doctors, and psychologists for decades to come.Part 2: How Media Sensationalism, Big Tech Bias Extended Lockdowns. Excerpt:
Epidemiologists created faulty lockdown models. The media promoted fear. Politicians assumed worst-case scenarios, and big tech suppressed dissenting views. This is how people’s fears grew disproportional to reality and how seemingly short-term lockdowns stretched into months.I’ll end these thoughts with a final quote from Israel’s Yoram Lass, who neatly summarized what just happened (and is still happening in many places):
It is what is known in science as positive feedback or a snowball effect. The government is afraid of its constituents. Therefore, it implements draconian measures. The constituents look at the draconian measures and become even more hysterical. They feed each other and the snowball becomes larger and larger until you reach irrational territory. This is nothing more than a flu epidemic if you care to look at the numbers and the data, but people who are in a state of anxiety are blind. If I were making the decisions, I would try to give people the real numbers. And I would never destroy my country.
Now what?
What should be done is so simple, IMO, but it never will, because too many people would have to admit they were wrong. But, I’ll say it anyway. My policy recommendation: remove 100% of newly created lockdown rules, secure nursing homes using Florida’s approach, tell everyone with an active COVID-19 infection to stay home until symptoms resolve or wear a mask if they need to go out in public, and encourage everyone else to wash their hands. Done deal.I saved one of my favorite quotes for last from Karolinska Institute’s Johan Giesecke (no surprise he’s Swedish), from an essay that appeared in early May in The Lancet:
These facts have led me to the following conclusions. Everyone will be exposed to severe acute respiratory syndrome coronavirus 2, and most people will become infected. COVID-19 is spreading like wildfire in all countries, but we do not see it—it almost always spreads from younger people with no or weak symptoms to other people who will also have mild symptoms. This is the real pandemic, but it goes on beneath the surface, and is probably at its peak now in many European countries. There is very little we can do to prevent this spread: a lockdown might delay severe cases for a while, but once restrictions are eased, cases will reappear. I expect that when we count the number of deaths from COVID-19 in each country in 1 year from now, the figures will be similar, regardless of measures taken.If you made it this far, thank you. You now share my burden in knowing the facts about Lockdown Lunacy. And, thank you to the many courageous medical professionals and scientists who are taking serious risk to their careers to publicly tell the truth.
Measures to flatten the curve might have an effect, but a lockdown only pushes the severe cases into the future —it will not prevent them. Admittedly, countries have managed to slow down spread so as not to overburden health-care systems, and, yes, effective drugs that save lives might soon be developed, but this pandemic is swift, and those drugs have to be developed, tested, and marketed quickly. Much hope is put in vaccines, but they will take time, and with the unclear protective immunological response to infection, it is not certain that vaccines will be very effective.
In summary, COVID-19 is a disease that is highly infectious and spreads rapidly through society. It is often quite symptomless and might pass unnoticed, but it also causes severe disease, and even death, in a proportion of the population, and our most important task is not to stop spread, which is all but futile, but to concentrate on giving the unfortunate victims optimal care.
**About the author: J.B. Handley is the best-selling author of How to End the Autism Epidemic. He graduated with honors from Stanford University, and currently serves as a Managing member of a private investment firm. He can be reached at jbhandleyblog@gmail.com

No comments:
Post a Comment